Ido Efrati
www.haaretz.com
Originally posted February 10, 2019
MDMA, popularly known as ecstasy, is a drug more commonly associated with raves and nightclubs than a therapist’s office.
Emerging research has shown promising results in using this “party drug” to treat patients suffering from post-traumatic stress disorder, and Israel’s Health Ministry has just approved the use of MDMA to treat dozens of patients.
MDMA is classified in Israel as a “dangerous drug”, recreational use is illegal, and therapeutic use of MDMA has yet to be formally approved and is still in clinical trials.
However, this treatment is deemed as “compassionate use,” which allows drugs that are still in development to be made available to patients outside of a clinical trial due to the lack of effective alternatives.
The info is here.
Welcome to the Nexus of Ethics, Psychology, Morality, Philosophy and Health Care
Welcome to the nexus of ethics, psychology, morality, technology, health care, and philosophy
Showing posts with label Treatment. Show all posts
Showing posts with label Treatment. Show all posts
Wednesday, March 20, 2019
Monday, March 11, 2019
The Parking Lot Suicide
Emily Wax-Thibodeaux.
The Washington Post
Originally published February 11, 2019
Here is an excerpt:
Miller was suffering from post-traumatic stress disorder and suicidal thoughts when he checked into the Minneapolis Department of Veterans Affairs hospital in February 2018. After spending four days in the mental-health unit, Miller walked to his truck in VA’s parking lot and shot himself in the very place he went to find help.
“The fact that my brother, Justin, never left the VA parking lot — it’s infuriating,” said Harrington, 37. “He did the right thing; he went in for help. I just can’t get my head around it.”
A federal investigation into Miller’s death found that the Minneapolis VA made multiple errors: not scheduling a follow-up appointment, failing to communicate with his family about the treatment plan and inadequately assessing his access to firearms.
Several days after his death, Miller’s parents received a package from the Department of Veterans Affairs — bottles of antidepressants and sleep aids prescribed to Miller.
His death is among 19 suicides that occurred on VA campuses from October 2017 to November 2018, seven of them in parking lots, according to the Department of Veterans Affairs.
While studies show that every suicide is highly complex — influenced by genetics, financial uncertainty, relationship loss and other factors — mental-health experts worry that veterans taking their lives on VA property has become a desperate form of protest against a system that some veterans feel hasn’t helped them.
The most recent parking lot suicide occurred weeks before Christmas in St. Petersburg, Fla. Marine Col. Jim Turner, 55, dressed in his uniform blues and medals, sat on top of his military and VA records and killed himself with a rifle outside the Bay Pines Department of Veterans Affairs.
“I bet if you look at the 22 suicides a day you will see VA screwed up in 90%,” Turner wrote in a note investigators found near his body.
The info is here.
The Washington Post
Originally published February 11, 2019
Here is an excerpt:
Miller was suffering from post-traumatic stress disorder and suicidal thoughts when he checked into the Minneapolis Department of Veterans Affairs hospital in February 2018. After spending four days in the mental-health unit, Miller walked to his truck in VA’s parking lot and shot himself in the very place he went to find help.
“The fact that my brother, Justin, never left the VA parking lot — it’s infuriating,” said Harrington, 37. “He did the right thing; he went in for help. I just can’t get my head around it.”
A federal investigation into Miller’s death found that the Minneapolis VA made multiple errors: not scheduling a follow-up appointment, failing to communicate with his family about the treatment plan and inadequately assessing his access to firearms.
Several days after his death, Miller’s parents received a package from the Department of Veterans Affairs — bottles of antidepressants and sleep aids prescribed to Miller.
His death is among 19 suicides that occurred on VA campuses from October 2017 to November 2018, seven of them in parking lots, according to the Department of Veterans Affairs.
While studies show that every suicide is highly complex — influenced by genetics, financial uncertainty, relationship loss and other factors — mental-health experts worry that veterans taking their lives on VA property has become a desperate form of protest against a system that some veterans feel hasn’t helped them.
The most recent parking lot suicide occurred weeks before Christmas in St. Petersburg, Fla. Marine Col. Jim Turner, 55, dressed in his uniform blues and medals, sat on top of his military and VA records and killed himself with a rifle outside the Bay Pines Department of Veterans Affairs.
“I bet if you look at the 22 suicides a day you will see VA screwed up in 90%,” Turner wrote in a note investigators found near his body.
The info is here.
Friday, March 1, 2019
Once-prominent 'conversion therapist' will now 'pursue life as a gay man'
Julie Compton
NBC News
Originally posted January 23, 2019
David Matheson, a once prominent Mormon “conversion therapist” who claims to have helped some gay men remain in heterosexual marriages, is looking for a boyfriend.
The revelation broke Sunday night after the LGBTQ nonprofit Truth Wins Out obtained a private Facebook post made by “conversion therapy” advocate Rich Wyler, which stated that Matheson “says that living a single, celibate life ‘just isn’t feasible for him,’ so he’s seeking a male partner.”
Matheson then confirmed Wyler’s assertions on Tuesday with a Facebook post of his own. “A year ago I realized I had to make substantial changes in my life. I realized I couldn’t stay in my marriage any longer. And I realized that it was time for me to affirm myself as gay,” he wrote.
Matheson, who was married to a woman for 34 years and is now divorced, also confirmed in an interview with NBC News that he is now dating men.
The info is here.
NBC News
Originally posted January 23, 2019
David Matheson, a once prominent Mormon “conversion therapist” who claims to have helped some gay men remain in heterosexual marriages, is looking for a boyfriend.
The revelation broke Sunday night after the LGBTQ nonprofit Truth Wins Out obtained a private Facebook post made by “conversion therapy” advocate Rich Wyler, which stated that Matheson “says that living a single, celibate life ‘just isn’t feasible for him,’ so he’s seeking a male partner.”
Matheson then confirmed Wyler’s assertions on Tuesday with a Facebook post of his own. “A year ago I realized I had to make substantial changes in my life. I realized I couldn’t stay in my marriage any longer. And I realized that it was time for me to affirm myself as gay,” he wrote.
Matheson, who was married to a woman for 34 years and is now divorced, also confirmed in an interview with NBC News that he is now dating men.
The info is here.
Tuesday, February 19, 2019
Even psychological placebos have an effect
University of Basel Press Release
Published February 5, 2019
Psychotherapy and placebos are both psychological interventions that not only have comparable effects, but that are also based on very similar mechanisms. Both forms of treatment are heavily influenced by the relationship between patients and those treating them, as well as by the expectations of recovery. Whereas placebo research mostly focuses on a biomedical model – an inert pill is provided with a medical rationale, which produces a corresponding effect – little is known about the effect of placebos provided with a psychological rationale.
“Green is calming”
Placebos can also have effects when specific psychological effects are attributed to them. This is the conclusion that researchers from the Division of Clinical Psychology and Psychotherapy at the University of Basel reached in three independent experiments with 421 healthy participants. The accompanying explanation – the narrative – played a key role when dispensing the placebos, as did the relationship between the researchers and the participants.
The researchers used the color green as the placebo in the video experiments, examining it both with and without a psychological narrative (“green is calming because it activates early conditioned emotional schemata”), as well as in the context of a neutral or a friendly relationship.
After viewing the videos, the participants assessed their subjective condition with questionnaires over several days. The results showed that the placebo had a positive effect on the participants’ well-being when it was prescribed together with a psychological narrative and in the context of a friendly relationship. The observed effect was strongest after administering the placebo but remained evident for up to one week.
Ethical implications
“The observed effects were comparable with those of psychotherapeutic interventions in the same populations,” says principal investigator Professor Jens Gaab. The fact that psychological placebos can have significant effects is not only important for understanding psychological interventions: “It challenges both research and clinical practice to address these mechanisms and effects, as well as their ethical implications.”
The pressor is here
Published February 5, 2019
Psychotherapy and placebos are both psychological interventions that not only have comparable effects, but that are also based on very similar mechanisms. Both forms of treatment are heavily influenced by the relationship between patients and those treating them, as well as by the expectations of recovery. Whereas placebo research mostly focuses on a biomedical model – an inert pill is provided with a medical rationale, which produces a corresponding effect – little is known about the effect of placebos provided with a psychological rationale.
“Green is calming”
Placebos can also have effects when specific psychological effects are attributed to them. This is the conclusion that researchers from the Division of Clinical Psychology and Psychotherapy at the University of Basel reached in three independent experiments with 421 healthy participants. The accompanying explanation – the narrative – played a key role when dispensing the placebos, as did the relationship between the researchers and the participants.
The researchers used the color green as the placebo in the video experiments, examining it both with and without a psychological narrative (“green is calming because it activates early conditioned emotional schemata”), as well as in the context of a neutral or a friendly relationship.
After viewing the videos, the participants assessed their subjective condition with questionnaires over several days. The results showed that the placebo had a positive effect on the participants’ well-being when it was prescribed together with a psychological narrative and in the context of a friendly relationship. The observed effect was strongest after administering the placebo but remained evident for up to one week.
Ethical implications
“The observed effects were comparable with those of psychotherapeutic interventions in the same populations,” says principal investigator Professor Jens Gaab. The fact that psychological placebos can have significant effects is not only important for understanding psychological interventions: “It challenges both research and clinical practice to address these mechanisms and effects, as well as their ethical implications.”
The pressor is here
Thursday, December 27, 2018
You Snooze, You Lose: Insurers Make The Old Adage Literally True
Justin Volz
ProPublica
Here is an excerpt:
In fact, faced with the popularity of CPAPs, which can cost $400 to $800, and their need for replacement filters, face masks and hoses, health insurers have deployed a host of tactics that can make the therapy more expensive or even price it out of reach.
Patients have been required to rent CPAPs at rates that total much more than the retail price of the devices, or they’ve discovered that the supplies would be substantially cheaper if they didn’t have insurance at all.
Experts who study health care costs say insurers’ CPAP strategies are part of the industry’s playbook of shifting the costs of widely used therapies, devices and tests to unsuspecting patients.
“The doctors and providers are not in control of medicine anymore,” said Harry Lawrence, owner of Advanced Oxy-Med Services, a New York company that provides CPAP supplies. “It’s strictly the insurance companies. They call the shots.”
Insurers say their concerns are legitimate. The masks and hoses can be cumbersome and noisy, and studies show that about third of patients don’t use their CPAPs as directed.
But the companies’ practices have spawned lawsuits and concerns by some doctors who say that policies that restrict access to the machines could have serious, or even deadly, consequences for patients with severe conditions. And privacy experts worry that data collected by insurers could be used to discriminate against patients or raise their costs.
The info is here.
ProPublica
Originally published November 21, 2018
Here is an excerpt:
In fact, faced with the popularity of CPAPs, which can cost $400 to $800, and their need for replacement filters, face masks and hoses, health insurers have deployed a host of tactics that can make the therapy more expensive or even price it out of reach.
Patients have been required to rent CPAPs at rates that total much more than the retail price of the devices, or they’ve discovered that the supplies would be substantially cheaper if they didn’t have insurance at all.
Experts who study health care costs say insurers’ CPAP strategies are part of the industry’s playbook of shifting the costs of widely used therapies, devices and tests to unsuspecting patients.
“The doctors and providers are not in control of medicine anymore,” said Harry Lawrence, owner of Advanced Oxy-Med Services, a New York company that provides CPAP supplies. “It’s strictly the insurance companies. They call the shots.”
Insurers say their concerns are legitimate. The masks and hoses can be cumbersome and noisy, and studies show that about third of patients don’t use their CPAPs as directed.
But the companies’ practices have spawned lawsuits and concerns by some doctors who say that policies that restrict access to the machines could have serious, or even deadly, consequences for patients with severe conditions. And privacy experts worry that data collected by insurers could be used to discriminate against patients or raise their costs.
The info is here.
Tuesday, November 27, 2018
A fate worse than death
Cathy Rentzenbrink
Prospect Magazine
Originally posted March 18, 2018
Here is an excerpt:
We have lost our way with death. Improvements in medicine have led us to believe that a long and fulfilling life is our birthright. Death is no longer seen as the natural consequence of life but as an inconvenient and unjust betrayal. We are in an age of denial.
Why does this matter? Why not allow ourselves this pleasant and surely harmless delusion? It matters because we are in a peculiar and precise period of history where our technological advances enable us to keep people alive when we probably shouldn’t. Life or death is no longer a black and white situation. There are many and various shades of grey. We behave as though death is the worst outcome, but it isn’t.
Many years after the accident, when I wrote a book about it called The Last Act of Love, I catalogued what happened to me as I witnessed the destruction of my brother. I detailed the drinking and the depression. The hardest thing was tracking our journey from hope to despair. I still find it hard to be precise about exactly when and how I realised that Matty would be better off dead. I know I moved from being convinced that if I tried hard enough I could bring Matty back to life, to thinking I should learn to love him as he was. Eventually I asked myself the right question: would Matty himself want to be alive like this? Of course, the answer was no.
The info is here.
Prospect Magazine
Originally posted March 18, 2018
Here is an excerpt:
We have lost our way with death. Improvements in medicine have led us to believe that a long and fulfilling life is our birthright. Death is no longer seen as the natural consequence of life but as an inconvenient and unjust betrayal. We are in an age of denial.
Why does this matter? Why not allow ourselves this pleasant and surely harmless delusion? It matters because we are in a peculiar and precise period of history where our technological advances enable us to keep people alive when we probably shouldn’t. Life or death is no longer a black and white situation. There are many and various shades of grey. We behave as though death is the worst outcome, but it isn’t.
Many years after the accident, when I wrote a book about it called The Last Act of Love, I catalogued what happened to me as I witnessed the destruction of my brother. I detailed the drinking and the depression. The hardest thing was tracking our journey from hope to despair. I still find it hard to be precise about exactly when and how I realised that Matty would be better off dead. I know I moved from being convinced that if I tried hard enough I could bring Matty back to life, to thinking I should learn to love him as he was. Eventually I asked myself the right question: would Matty himself want to be alive like this? Of course, the answer was no.
The info is here.
Wednesday, November 7, 2018
Hospitals are fed up with drug companies, so they’re starting their own
 Carolyn Johnson
Carolyn JohnsonThe Washington Post
Originally posted September 6, 2018
A group of major American hospitals, battered by price spikes on old drugs and long-lasting shortages of critical medicines, has launched a mission-driven, not-for-profit generic drug company, Civica Rx, to take some control over the drug supply.
Backed by seven large health systems and three philanthropic groups, the new venture will be led by an industry insider who refuses to draw a salary. The company will focus initially on establishing price transparency and stable supplies for 14 generic drugs used in hospitals, without pressure from shareholders to issue dividends or push a stock price higher.
“We’re trying to do the right thing — create a first-of-its-kind societal asset with one mission: to make sure essential generic medicines are affordable and available to everyone,” said Dan Liljenquist, chair of Civica Rx and chief strategy officer at Intermountain Healthcare in Utah.
The consortium, which includes health systems such as the Mayo Clinic and HCA Healthcare, collectively represents about 500 hospitals. Liljenquist said that the initial governing members have already committed $100 million to the effort. The business model will ultimately rely on the long-term contracts that member health care organizations agree to — a commitment to buy a fixed portion of their drug volume from Civica.
The info is here.
Friday, November 2, 2018
Companies Tout Psychiatric Pharmacogenomic Testing, But Is It Ready for a Store Near You?
Jennifer Abbasi
JAMA Network
Originally posted October 3, 2018
Here is an excerpt:
According to Dan Dowd, PharmD, vice president of medical affairs at Genomind, pharmacists in participating stores can inform customers about the Genecept Assay if they notice a history of psychotropic drug switching or drug-related adverse effects. If the test is administered, a physician’s order is required for the company’s laboratory to process it.
“This certainly is a recipe for selling a whole lot more tests,” Potash said of the approach, adding that patients often feel “desperate” to find a successful treatment. “What percentage of the time selling these tests will result in better patient outcomes remains to be seen.”
Biernacka also had reservations about the in-store model. “Generally, it could be helpful for a pharmacist to tell a patient or their provider that perhaps the patient could benefit from pharmacogenetic testing,” she said. “[B]ut until the tests are more thoroughly assessed, the decision to pursue such an option (and with which test) should be left more to the treating clinician and patient.”
Some physicians said they’ve found pharmacogenomic testing to be useful. Aron Fast, MD, a family physician in Hesston, Kansas, uses GeneSight for patients with depression or anxiety who haven’t improved after trying 2 or 3 antidepressants. Each time, he said, his patients were less depressed or anxious after switching to a new drug based on their genotyping results.
Part of their improvements may stem from expecting the test to help, he acknowledged. The testing “raises confidence in the medication to be prescribed,” Müller explained, which might contribute to a placebo effect. However, Müller emphasized that the placebo effect alone is unlikely to explain lasting improvements in patients with moderate to severe depression. In his psychiatric consulting practice, pharmacogenomic-guided drug changes have led to improvements in patients “sometimes even up to the point where they’re completely remitted,” he said.
The info is here.
JAMA Network
Originally posted October 3, 2018
Here is an excerpt:
According to Dan Dowd, PharmD, vice president of medical affairs at Genomind, pharmacists in participating stores can inform customers about the Genecept Assay if they notice a history of psychotropic drug switching or drug-related adverse effects. If the test is administered, a physician’s order is required for the company’s laboratory to process it.
“This certainly is a recipe for selling a whole lot more tests,” Potash said of the approach, adding that patients often feel “desperate” to find a successful treatment. “What percentage of the time selling these tests will result in better patient outcomes remains to be seen.”
Biernacka also had reservations about the in-store model. “Generally, it could be helpful for a pharmacist to tell a patient or their provider that perhaps the patient could benefit from pharmacogenetic testing,” she said. “[B]ut until the tests are more thoroughly assessed, the decision to pursue such an option (and with which test) should be left more to the treating clinician and patient.”
Some physicians said they’ve found pharmacogenomic testing to be useful. Aron Fast, MD, a family physician in Hesston, Kansas, uses GeneSight for patients with depression or anxiety who haven’t improved after trying 2 or 3 antidepressants. Each time, he said, his patients were less depressed or anxious after switching to a new drug based on their genotyping results.
Part of their improvements may stem from expecting the test to help, he acknowledged. The testing “raises confidence in the medication to be prescribed,” Müller explained, which might contribute to a placebo effect. However, Müller emphasized that the placebo effect alone is unlikely to explain lasting improvements in patients with moderate to severe depression. In his psychiatric consulting practice, pharmacogenomic-guided drug changes have led to improvements in patients “sometimes even up to the point where they’re completely remitted,” he said.
The info is here.
Friday, October 19, 2018
Risk Management Considerations When Treating Violent Patients
Kristen Lambert
Psychiatric News
Originally posted September 4, 2018
Here is an excerpt:
When a patient has a history of expressing homicidal ideation or has been violent previously, you should document, in every subsequent session, whether the patient admits or denies homicidal ideation. When the patient expresses homicidal ideation, document what he/she expressed and the steps you did or did not take in response and why. Should an incident occur, your documentation will play an important role in defending your actions.
Despite taking precautions, your patient may still commit a violent act. The following are some strategies that may minimize your risk.
Psychiatric News
Originally posted September 4, 2018
Here is an excerpt:
When a patient has a history of expressing homicidal ideation or has been violent previously, you should document, in every subsequent session, whether the patient admits or denies homicidal ideation. When the patient expresses homicidal ideation, document what he/she expressed and the steps you did or did not take in response and why. Should an incident occur, your documentation will play an important role in defending your actions.
Despite taking precautions, your patient may still commit a violent act. The following are some strategies that may minimize your risk.
- Conduct complete timely/thorough risk assessments.
- Document, including the reasons for taking and not taking certain actions.
- Understand your state’s law on duty to warn. Be aware of the language in the law on whether you have a mandatory, permissive, or no duty to warn/protect.
- Understand your state’s laws regarding civil commitment.
- Understand your state’s laws regarding disclosure of confidential information and when you can do so.
- Understand your state’s laws regarding discussing firearms ownership and/or possession with patients.
- If you have questions, consult an attorney or risk management professional.
Wednesday, October 10, 2018
Psychologists Are Standing Up Against Torture at Gitmo
 Rebecca Gordon
Rebecca GordontheNation.com
Originally posted September 11, 2018
Sometimes the good guys do win. That’s what happened on August 8 in San Francisco when the Council of Representatives of the American Psychological Association (APA) decided to extend a policy keeping its members out of the US detention center at Guantánamo Bay, Cuba.
The APA’s decision is important—and not just symbolically. Today we have a president who has promised to bring back torture and “load up” Guantánamo “with some bad dudes.” When healing professionals refuse to work there, they are standing up for human rights and against torture.
It wasn’t always so. In the early days of Guantánamo, military psychologists contributed to detainee interrogations there. It was for Guantánamo that Defense Secretary Donald Rumsfeld approved multiple torture methods, including among others excruciating stress positions, prolonged isolation, sensory deprivation, and enforced nudity. Military psychologists advised on which techniques would take advantage of the weaknesses of individual detainees. And it was two psychologists, one an APA member, who designed the CIA’s whole “enhanced interrogation program.”
The info is here.
Monday, October 1, 2018
How Do Medicalization and Rescue Fantasy Prevent Healthy Dying?
Peter T. Hetzler III and Lydia S. Dugdale
AMA Journal of Ethics
2018;20(8):E766-773.
Abstract
Before antibiotics, cardiopulmonary resuscitation (CPR), and life-sustaining technologies, humans had little choice about the timing and manner of their deaths. Today, the medicalization of death has enabled patients to delay death, prolonging their living and dying. New technology, the influence of the media, and medical professionals themselves have together transformed dying from a natural part of the human experience into a medical crisis from which a patient must be rescued, often through the aggressive extension of life or through its premature termination. In this paper, we examine problematic forms of rescue medicine and suggest the need to rethink medicalized dying within the context of medicine’s orientation to health and wholeness.
The info is here.
AMA Journal of Ethics
2018;20(8):E766-773.
Abstract
Before antibiotics, cardiopulmonary resuscitation (CPR), and life-sustaining technologies, humans had little choice about the timing and manner of their deaths. Today, the medicalization of death has enabled patients to delay death, prolonging their living and dying. New technology, the influence of the media, and medical professionals themselves have together transformed dying from a natural part of the human experience into a medical crisis from which a patient must be rescued, often through the aggressive extension of life or through its premature termination. In this paper, we examine problematic forms of rescue medicine and suggest the need to rethink medicalized dying within the context of medicine’s orientation to health and wholeness.
The info is here.
Wednesday, September 26, 2018
Do psychotropic drugs enhance, or diminish, human agency?
Rami Gabriel
aeon.co
Originally posted September 3, 2018
Here is an excerpt:
Psychological medications such as Xanax, Ritalin and aspirin help to modify undesirable behaviours, thought patterns and the perception of pain. They purport to treat the underlying chemical cause rather than the social, interpersonal or psychodynamic causes of pathology. Self-knowledge gained by introspection and dialogue are no longer our primary means for modifying psychological states. By prescribing such medication, physicians are implicitly admitting that cognitive and behavioural training is insufficient and impractical, and that ‘the brain’, of which nonspecialists have little explicit understanding, is in fact the level where errors occur. Indeed, drugs are reliable and effective because they implement the findings of neuroscience and supplement (or in many cases substitute for) our humanist discourse about self-development and agency. In using such drugs, we become transhuman hybrid beings who build tools into the regulatory plant of the body.
Recreational drugs, on the other hand, are essentially hedonic tools that allow for stress-release and the diminishment of inhibition and sense of responsibility. Avenues of escape are reached through derangement of thought and perception; many find pleasure in this transcendence of quotidian experience and transgression of social norms. There is also a Dionysian, or spiritual, purpose to recreational inebriation, which can enable revelations that enhance intimacy and the emotional need for existential reflection. Here drugs act as portals into spiritual rituals and otherwise restricted metaphysical spaces. The practice of imbibing a sacred substance is as old as ascetic and mindfulness practices but, in our times, drugs are overwhelmingly the most commonly used tool for tending to this element of the human condition.
The info is here.
aeon.co
Originally posted September 3, 2018
Here is an excerpt:
Psychological medications such as Xanax, Ritalin and aspirin help to modify undesirable behaviours, thought patterns and the perception of pain. They purport to treat the underlying chemical cause rather than the social, interpersonal or psychodynamic causes of pathology. Self-knowledge gained by introspection and dialogue are no longer our primary means for modifying psychological states. By prescribing such medication, physicians are implicitly admitting that cognitive and behavioural training is insufficient and impractical, and that ‘the brain’, of which nonspecialists have little explicit understanding, is in fact the level where errors occur. Indeed, drugs are reliable and effective because they implement the findings of neuroscience and supplement (or in many cases substitute for) our humanist discourse about self-development and agency. In using such drugs, we become transhuman hybrid beings who build tools into the regulatory plant of the body.
Recreational drugs, on the other hand, are essentially hedonic tools that allow for stress-release and the diminishment of inhibition and sense of responsibility. Avenues of escape are reached through derangement of thought and perception; many find pleasure in this transcendence of quotidian experience and transgression of social norms. There is also a Dionysian, or spiritual, purpose to recreational inebriation, which can enable revelations that enhance intimacy and the emotional need for existential reflection. Here drugs act as portals into spiritual rituals and otherwise restricted metaphysical spaces. The practice of imbibing a sacred substance is as old as ascetic and mindfulness practices but, in our times, drugs are overwhelmingly the most commonly used tool for tending to this element of the human condition.
The info is here.
Tuesday, September 25, 2018
Horrific deaths, brutal treatment: Mental illness in America’s jails
Gary A. Harki
The Virginian-Pilot
Originally published August 23, 2018
Here is an excerpt:
“We are arresting people who have no idea what the laws are or the rules are because they're off their medications,” said Nashville Sheriff Daron Hall, a vice president of the National Sheriffs’ Association. “You'd never arrest someone for a heart attack, but you're comfortable arresting someone who is diagnosed mentally ill. No other country in the world is doing it this way.”
In addition to causing pain and suffering for people with mental illness, the practice is costing municipalities millions.
At least 53 percent of the deaths examined have resulted in a lawsuit. Combined, the cases have cost municipalities at least $145 million. The true cost is much higher – in many cases, lawsuits are still pending and in others the settlement amount is secret. The figures also do not take into account lawyers’ fees.
The article is here.
There are a series of articles related to mental health issues in prison.
The Virginian-Pilot
Originally published August 23, 2018
Here is an excerpt:
“We are arresting people who have no idea what the laws are or the rules are because they're off their medications,” said Nashville Sheriff Daron Hall, a vice president of the National Sheriffs’ Association. “You'd never arrest someone for a heart attack, but you're comfortable arresting someone who is diagnosed mentally ill. No other country in the world is doing it this way.”
In addition to causing pain and suffering for people with mental illness, the practice is costing municipalities millions.
At least 53 percent of the deaths examined have resulted in a lawsuit. Combined, the cases have cost municipalities at least $145 million. The true cost is much higher – in many cases, lawsuits are still pending and in others the settlement amount is secret. The figures also do not take into account lawyers’ fees.
The article is here.
There are a series of articles related to mental health issues in prison.
Wednesday, September 19, 2018
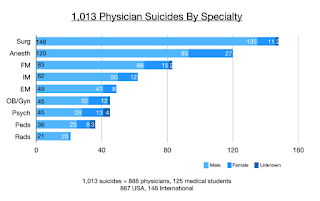
Why “happy” doctors die by suicide
 Pamela Wible
Pamela Wiblewww.idealmedicalcare.org
Originally posted on August 24, 2018
Here is an excerpt:
Doctor suicides on the registry were submitted to me during a six-year period (2012-2018) by families, friends, and colleagues who knew the deceased. After speaking to thousands of suicidal physicians since 2012 on my informal doctor suicide hotline and analyzing registry data, I discovered surprising themes—many unique to physicians.
Public perception maintains that doctors are successful, intelligent, wealthy, and immune from the problems of the masses. To patients, it is inconceivable that doctors would have the highest suicide rate of any profession (5).
Even more baffling, “happy” doctors are dying by suicide. Many doctors who kill themselves appear to be the most optimistic, upbeat, and confident people. Just back from Disneyland, just bought tickets for a family cruise, just gave a thumbs up to the team after a successful surgery—and hours later they shoot themselves in the head.
Doctors are masters of disguise and compartmentalization.
Turns out some of the happiest people—especially those who spend their days making other people happy—may be masking their own despair.
The info is here.
Thursday, September 13, 2018
How Should Clinicians Respond to Requests from Patients to Participate in Prayer?
 A. R. Christensen, T. E. Cook, and R. M. Arnold
A. R. Christensen, T. E. Cook, and R. M. ArnoldAMA J Ethics. 2018;20(7):E621-629.
Abstract
Over the past 20 years, physicians have shifted from viewing a patient’s request for prayer as a violation of professional boundaries to a question deserving nuanced understanding of the patient’s needs and the clinician’s boundaries. In this case, Mrs. C’s request for prayer can reflect religious distress, anxiety about her clinical circumstances, or a desire to better connect with her physician. These different needs suggest that it is important to understand the request before responding. To do this well requires that Dr. Q not be emotionally overwhelmed by the request and that she has skill in discerning potential reasons for the request.
The info is here.
Meet the Chatbots Providing Mental Health Care
Daniela Hernandez
Wall Street Journal
Originally published Aug. 9, 2018
Here is an excerpt:
Wysa Ltd., a London- and Bangalore-based startup, is testing a free chatbot to teach adolescents emotional resilience, said co-founder Ramakant Vempati. In the app, a chubby penguin named Wysa helps users evaluate the sources of their stress and provides tips on how to stay positive, like thinking of a loved one or spending time outside. The company said its 400,000 users, most of whom are under 35, have had more than 20 million conversations with the bot.
Wysa is a wellness app, not a medical intervention, Vempati said, but it relies on cognitive behavioral therapy, mindfulness techniques and meditations that are “known to work in a self-help context.” If a user expresses thoughts of self-harm, Wysa reminds them that it’s just a bot and provides contact information for crisis hotlines. Alternatively, for $30 a month, users can access unlimited chat sessions with a human “coach.” Other therapy apps, such as Talkspace, offer similar low-cost services with licensed professionals.
Chatbots have potential, said Beth Jaworski, a mobile apps specialist at the National Center for PTSD in Menlo Park, Calif. But definitive research on whether they can help patients with more serious conditions, like major depression, still hasn’t been done, in part because the technology is so new, she said. Clinicians also worry about privacy. Mental health information is sensitive data; turning it over to companies could have unforeseen consequences.
The article is here.
Wall Street Journal
Originally published Aug. 9, 2018
Here is an excerpt:
Wysa Ltd., a London- and Bangalore-based startup, is testing a free chatbot to teach adolescents emotional resilience, said co-founder Ramakant Vempati. In the app, a chubby penguin named Wysa helps users evaluate the sources of their stress and provides tips on how to stay positive, like thinking of a loved one or spending time outside. The company said its 400,000 users, most of whom are under 35, have had more than 20 million conversations with the bot.
Wysa is a wellness app, not a medical intervention, Vempati said, but it relies on cognitive behavioral therapy, mindfulness techniques and meditations that are “known to work in a self-help context.” If a user expresses thoughts of self-harm, Wysa reminds them that it’s just a bot and provides contact information for crisis hotlines. Alternatively, for $30 a month, users can access unlimited chat sessions with a human “coach.” Other therapy apps, such as Talkspace, offer similar low-cost services with licensed professionals.
Chatbots have potential, said Beth Jaworski, a mobile apps specialist at the National Center for PTSD in Menlo Park, Calif. But definitive research on whether they can help patients with more serious conditions, like major depression, still hasn’t been done, in part because the technology is so new, she said. Clinicians also worry about privacy. Mental health information is sensitive data; turning it over to companies could have unforeseen consequences.
The article is here.
Monday, September 10, 2018
Cognitive Biases Tricking Your Brain
 Ben Yagoda
Ben YagodaThe Atlantic
September 2018 Issue
Here is an excerpt:
Because biases appear to be so hardwired and inalterable, most of the attention paid to countering them hasn’t dealt with the problematic thoughts, judgments, or predictions themselves. Instead, it has been devoted to changing behavior, in the form of incentives or “nudges.” For example, while present bias has so far proved intractable, employers have been able to nudge employees into contributing to retirement plans by making saving the default option; you have to actively take steps in order to not participate. That is, laziness or inertia can be more powerful than bias. Procedures can also be organized in a way that dissuades or prevents people from acting on biased thoughts. A well-known example: the checklists for doctors and nurses put forward by Atul Gawande in his book The Checklist Manifesto.
Is it really impossible, however, to shed or significantly mitigate one’s biases? Some studies have tentatively answered that question in the affirmative. These experiments are based on the reactions and responses of randomly chosen subjects, many of them college undergraduates: people, that is, who care about the $20 they are being paid to participate, not about modifying or even learning about their behavior and thinking. But what if the person undergoing the de-biasing strategies was highly motivated and self-selected? In other words, what if it was me?
The info is here.
Thursday, August 23, 2018
Implicit Bias in Patient Care: An Endemic Blight on Quality Care
JoAnn Grif Alspach
Critical Care Nurse
August 2018 vol. 38 no. 4 12-16
Here is an excerpt:
How Implicit Bias Is Manifested
A systematic review by Hall and colleagues revealed that implicit bias is manifested in 4 key areas: patient-provider interactions, treatment decisions, treatment adherence, and patient health outcomes. How a physician communicates, including verbal cues, body language, and nonverbal behavior (physical proximity, frequency of eye contact) may manifest subconscious bias.7,10 Several investigators found evidence that providers interact more effectively with white than nonwhite patients. Bias may affect the nature and extent of diagnostic assessments and the range and scope of therapies considered. Nonwhite patients receive fewer cardiovascular interventions and kidney transplants. One meta-analysis found that 20 of 25 assumption method studies demonstrated bias either in the diagnosis, treatment recommendations, number of questions asked, or tests ordered. Women are 3 times less likely than men to receive knee arthroplasty despite comparable indications. Bias can detrimentally affect whether patients seek or return for care, follow treatment protocols, and, perhaps cumulatively, can influence outcomes of care. Numerous research studies offer evidence that implicit bias is associated with higher complication rates, greater morbidity, and higher patient mortality.
The info is here.
Critical Care Nurse
August 2018 vol. 38 no. 4 12-16
Here is an excerpt:
How Implicit Bias Is Manifested
A systematic review by Hall and colleagues revealed that implicit bias is manifested in 4 key areas: patient-provider interactions, treatment decisions, treatment adherence, and patient health outcomes. How a physician communicates, including verbal cues, body language, and nonverbal behavior (physical proximity, frequency of eye contact) may manifest subconscious bias.7,10 Several investigators found evidence that providers interact more effectively with white than nonwhite patients. Bias may affect the nature and extent of diagnostic assessments and the range and scope of therapies considered. Nonwhite patients receive fewer cardiovascular interventions and kidney transplants. One meta-analysis found that 20 of 25 assumption method studies demonstrated bias either in the diagnosis, treatment recommendations, number of questions asked, or tests ordered. Women are 3 times less likely than men to receive knee arthroplasty despite comparable indications. Bias can detrimentally affect whether patients seek or return for care, follow treatment protocols, and, perhaps cumulatively, can influence outcomes of care. Numerous research studies offer evidence that implicit bias is associated with higher complication rates, greater morbidity, and higher patient mortality.
The info is here.
Monday, August 13, 2018
This AI Just Beat Human Doctors On A Clinical Exam
Parmy Olson
Forbes.com
Originally posted June 28, 2018
Here is an excerpt:
Now Parsa is bringing his software service and virtual doctor network to insurers in the U.S. His pitch is that the smarter and more “reassuring” his AI-powered chatbot gets, the more likely patients across the Atlantic are to resolve their issues with software alone.
It’s a model that could save providers millions, potentially, but Parsa has yet to secure a big-name American customer.
“The American market is much more tuned to the economics of healthcare,” he said from his office. “We’re talking to everyone: insurers, employers, health systems. They have massive gaps in delivery of the care.”
“We will set up physical and virtual clinics, and AI services in the United States,” he said, adding that Babylon would be operational with U.S. clinics in 2019, starting state by state. “For a fixed fee, we take total responsibility for the cost of primary care.”
Parsa isn’t shy about his transatlantic ambitions: “I think the U.S. will be our biggest market shortly,” he adds.
The info is here.
Forbes.com
Originally posted June 28, 2018
Here is an excerpt:
Now Parsa is bringing his software service and virtual doctor network to insurers in the U.S. His pitch is that the smarter and more “reassuring” his AI-powered chatbot gets, the more likely patients across the Atlantic are to resolve their issues with software alone.
It’s a model that could save providers millions, potentially, but Parsa has yet to secure a big-name American customer.
“The American market is much more tuned to the economics of healthcare,” he said from his office. “We’re talking to everyone: insurers, employers, health systems. They have massive gaps in delivery of the care.”
“We will set up physical and virtual clinics, and AI services in the United States,” he said, adding that Babylon would be operational with U.S. clinics in 2019, starting state by state. “For a fixed fee, we take total responsibility for the cost of primary care.”
Parsa isn’t shy about his transatlantic ambitions: “I think the U.S. will be our biggest market shortly,” he adds.
The info is here.
Wednesday, July 11, 2018
Could Moral Enhancement Interventions be Medically Indicated?
Sarah Carter
Health Care Analysis
December 2017, Volume 25, Issue 4, pp 338–353
Abstract
This paper explores the position that moral enhancement interventions could be medically indicated (and so considered therapeutic) in cases where they provide a remedy for a lack of empathy, when such a deficit is considered pathological. In order to argue this claim, the question as to whether a deficit of empathy could be considered to be pathological is examined, taking into account the difficulty of defining illness and disorder generally, and especially in the case of mental health. Following this, Psychopathy and a fictionalised mental disorder (Moral Deficiency Disorder) are explored with a view to consider moral enhancement techniques as possible treatments for both conditions. At this juncture, having asserted and defended the position that moral enhancement interventions could, under certain circumstances, be considered medically indicated, this paper then goes on to briefly explore some of the consequences of this assertion. First, it is acknowledged that this broadening of diagnostic criteria in light of new interventions could fall foul of claims of medicalisation. It is then briefly noted that considering moral enhancement technologies to be akin to therapies in certain circumstances could lead to ethical and legal consequences and questions, such as those regarding regulation, access, and even consent.
The paper is here.
Health Care Analysis
December 2017, Volume 25, Issue 4, pp 338–353
Abstract
This paper explores the position that moral enhancement interventions could be medically indicated (and so considered therapeutic) in cases where they provide a remedy for a lack of empathy, when such a deficit is considered pathological. In order to argue this claim, the question as to whether a deficit of empathy could be considered to be pathological is examined, taking into account the difficulty of defining illness and disorder generally, and especially in the case of mental health. Following this, Psychopathy and a fictionalised mental disorder (Moral Deficiency Disorder) are explored with a view to consider moral enhancement techniques as possible treatments for both conditions. At this juncture, having asserted and defended the position that moral enhancement interventions could, under certain circumstances, be considered medically indicated, this paper then goes on to briefly explore some of the consequences of this assertion. First, it is acknowledged that this broadening of diagnostic criteria in light of new interventions could fall foul of claims of medicalisation. It is then briefly noted that considering moral enhancement technologies to be akin to therapies in certain circumstances could lead to ethical and legal consequences and questions, such as those regarding regulation, access, and even consent.
The paper is here.
Subscribe to:
Posts (Atom)