Donovan Slack
USA Today
Originally published December 21, 2017
The Department of Veterans Affairs has allowed its hospitals across the country to hire health care providers with revoked medical licenses for at least 15 years in violation of federal law, a USA TODAY investigation found.
The VA issued national guidelines in 2002 giving local hospitals discretion to hire clinicians after “prior consideration of all relevant facts surrounding” any revocations and as long as they still had a license in one state.
But a federal law passed in 1999 bars the VA from employing any health care worker whose license has been yanked by any state.
Hospital officials at the VA in Iowa City relied on the illegal guidance earlier this year to hire neurosurgeon John Henry Schneider, who had revealed in his application that he had numerous malpractice claims and settlements and Wyoming had revoked his license after a patient death. He still had a license in Montana.
The article is here.
Welcome to the Nexus of Ethics, Psychology, Morality, Philosophy and Health Care
Welcome to the nexus of ethics, psychology, morality, technology, health care, and philosophy
Showing posts with label Fidelity. Show all posts
Showing posts with label Fidelity. Show all posts
Wednesday, January 3, 2018
Monday, December 18, 2017
Unconscious Patient With 'Do Not Resuscitate' Tattoo Causes Ethical Conundrum at Hospital
George Dvorsky
Gizmodo
Originally published November 30, 2017
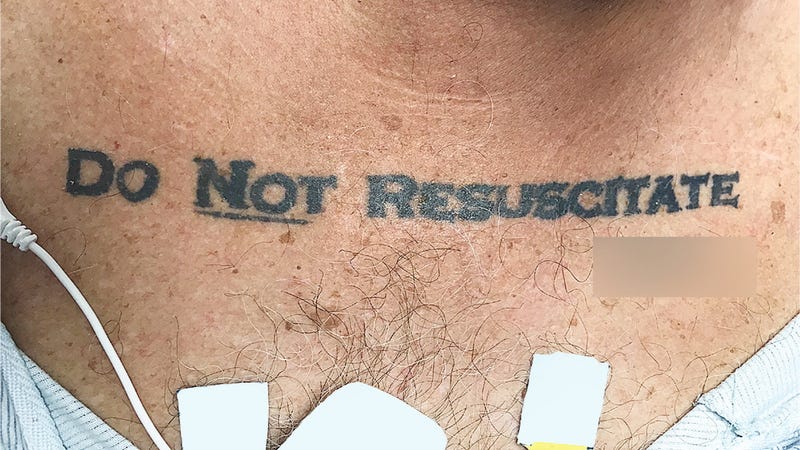 When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.
When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.
But with the “DO NOT RESUSCITATE” tattoo glaring back at them, the ICU team was suddenly confronted with a serious dilemma. The patient arrived at the hospital without ID, the medical staff was unable to contact next of kin, and efforts to revive or communicate with the patient were futile. The medical staff had no way of knowing if the tattoo was representative of the man’s true end-of-life wishes, so they decided to play it safe and ignore it.
The article is here.
Gizmodo
Originally published November 30, 2017
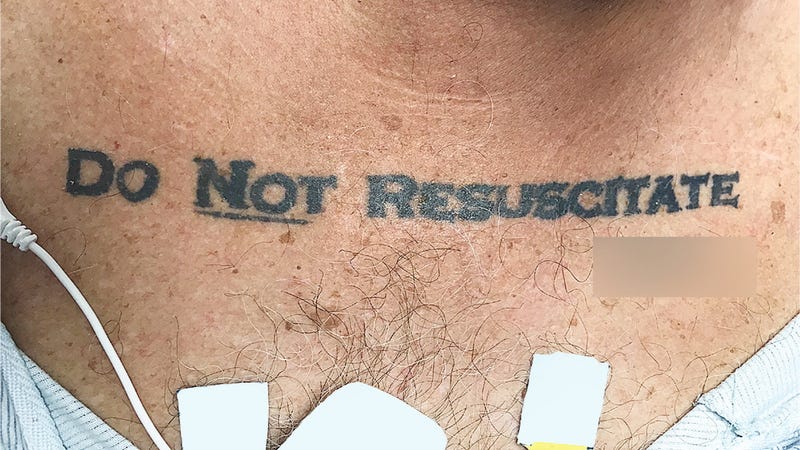 When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.
When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.But with the “DO NOT RESUSCITATE” tattoo glaring back at them, the ICU team was suddenly confronted with a serious dilemma. The patient arrived at the hospital without ID, the medical staff was unable to contact next of kin, and efforts to revive or communicate with the patient were futile. The medical staff had no way of knowing if the tattoo was representative of the man’s true end-of-life wishes, so they decided to play it safe and ignore it.
The article is here.
Wednesday, December 6, 2017
Disturbing allegations against psychologist at VT treatment center
Jennifer Costa
WCAX.com
Originally published November 17, 2017
Here is an excerpt:
Simonds is accused making comments about female patients, calling them "whores" or saying they look "sexy" and asking inappropriate details about their sex lives. Staff members allege he showed young women favoritism, made promises about drug treatment and bypassed waiting lists to get them help ahead of others.
He's accused of yelling and physically intimidating patients. Some refused to file complaints fearing he would pull their treatment opportunities.
Staffers go on to paint a nasty picture of their work environment, telling the state Simonds routinely threatened, cursed and yelled at them, calling them derogatory names like "retarded," "monkeys," "fat and lazy," and threatening to fire them at will while sexually harassing female subordinates.
Co-workers claim Simonds banned them from referring residential patients to facilities closer to their homes, instructed them to alter referrals to keep them in the Maple Leaf system and fired a clinician who refused to follow these orders. He is also accused of telling staff members to lie to the state about staffing to maintain funding and of directing clinicians to keep patients longer than necessary to drum up revenue.
The article is here.
WCAX.com
Originally published November 17, 2017
Here is an excerpt:
Simonds is accused making comments about female patients, calling them "whores" or saying they look "sexy" and asking inappropriate details about their sex lives. Staff members allege he showed young women favoritism, made promises about drug treatment and bypassed waiting lists to get them help ahead of others.
He's accused of yelling and physically intimidating patients. Some refused to file complaints fearing he would pull their treatment opportunities.
Staffers go on to paint a nasty picture of their work environment, telling the state Simonds routinely threatened, cursed and yelled at them, calling them derogatory names like "retarded," "monkeys," "fat and lazy," and threatening to fire them at will while sexually harassing female subordinates.
Co-workers claim Simonds banned them from referring residential patients to facilities closer to their homes, instructed them to alter referrals to keep them in the Maple Leaf system and fired a clinician who refused to follow these orders. He is also accused of telling staff members to lie to the state about staffing to maintain funding and of directing clinicians to keep patients longer than necessary to drum up revenue.
The article is here.
Monday, October 16, 2017
Can we teach robots ethics?
Dave Edmonds
BBC.com
Originally published October 15, 2017
Here is an excerpt:
However machine learning throws up problems of its own. One is that the machine may learn the wrong lessons. To give a related example, machines that learn language from mimicking humans have been shown to import various biases. Male and female names have different associations. The machine may come to believe that a John or Fred is more suitable to be a scientist than a Joanna or Fiona. We would need to be alert to these biases, and to try to combat them.
A yet more fundamental challenge is that if the machine evolves through a learning process we may be unable to predict how it will behave in the future; we may not even understand how it reaches its decisions. This is an unsettling possibility, especially if robots are making crucial choices about our lives. A partial solution might be to insist that if things do go wrong, we have a way to audit the code - a way of scrutinising what's happened. Since it would be both silly and unsatisfactory to hold the robot responsible for an action (what's the point of punishing a robot?), a further judgement would have to be made about who was morally and legally culpable for a robot's bad actions.
One big advantage of robots is that they will behave consistently. They will operate in the same way in similar situations. The autonomous weapon won't make bad choices because it is angry. The autonomous car won't get drunk, or tired, it won't shout at the kids on the back seat. Around the world, more than a million people are killed in car accidents each year - most by human error. Reducing those numbers is a big prize.
The article is here.
BBC.com
Originally published October 15, 2017
Here is an excerpt:
However machine learning throws up problems of its own. One is that the machine may learn the wrong lessons. To give a related example, machines that learn language from mimicking humans have been shown to import various biases. Male and female names have different associations. The machine may come to believe that a John or Fred is more suitable to be a scientist than a Joanna or Fiona. We would need to be alert to these biases, and to try to combat them.
A yet more fundamental challenge is that if the machine evolves through a learning process we may be unable to predict how it will behave in the future; we may not even understand how it reaches its decisions. This is an unsettling possibility, especially if robots are making crucial choices about our lives. A partial solution might be to insist that if things do go wrong, we have a way to audit the code - a way of scrutinising what's happened. Since it would be both silly and unsatisfactory to hold the robot responsible for an action (what's the point of punishing a robot?), a further judgement would have to be made about who was morally and legally culpable for a robot's bad actions.
One big advantage of robots is that they will behave consistently. They will operate in the same way in similar situations. The autonomous weapon won't make bad choices because it is angry. The autonomous car won't get drunk, or tired, it won't shout at the kids on the back seat. Around the world, more than a million people are killed in car accidents each year - most by human error. Reducing those numbers is a big prize.
The article is here.
Saturday, July 29, 2017
Trump Has Plunged Nation Into ‘Ethics Crisis,’ Ex-Watchdog Says
Britain Eakin
Courthouse News Service
Originally published July 28, 2017
The government’s former top ethics chief sounded the alarm Friday, saying the first eight months of the Trump administration have been “an absolute shock to the system” that has plunged the nation into “an ethics crisis.”
Walter Shaub Jr. resigned July 6 after months of clashes with the White House over issues such as President Trump’s refusal to divest his businesses and the administration’s delay in disclosing ethics waivers for appointees.
As he left office he told NPR that “the current situation has made it clear that the ethics program needs to be stronger than it is.”
He did not elaborate at that time on what about the “situation” so troubled him, but he said at the Campaign Legal Center, he would have more freedom “to push for reform” while broadening his focus to ethics issues at all levels of government.
During a talk at the National Press Club Friday morning, Shaub said the president and other administration officials have departed from ethical principles and norms as part of a broader assault on the American representative form of government.
Shaub said he is “extremely concerned” by this.
“The biggest concern is that norms evolve. So if we have a shock to the system, what we’re experiencing now could become the new norm,” Shaub said.
The article is here.
Courthouse News Service
Originally published July 28, 2017
The government’s former top ethics chief sounded the alarm Friday, saying the first eight months of the Trump administration have been “an absolute shock to the system” that has plunged the nation into “an ethics crisis.”
Walter Shaub Jr. resigned July 6 after months of clashes with the White House over issues such as President Trump’s refusal to divest his businesses and the administration’s delay in disclosing ethics waivers for appointees.
As he left office he told NPR that “the current situation has made it clear that the ethics program needs to be stronger than it is.”
He did not elaborate at that time on what about the “situation” so troubled him, but he said at the Campaign Legal Center, he would have more freedom “to push for reform” while broadening his focus to ethics issues at all levels of government.
During a talk at the National Press Club Friday morning, Shaub said the president and other administration officials have departed from ethical principles and norms as part of a broader assault on the American representative form of government.
Shaub said he is “extremely concerned” by this.
“The biggest concern is that norms evolve. So if we have a shock to the system, what we’re experiencing now could become the new norm,” Shaub said.
The article is here.
Thursday, December 15, 2016
How Well Does Your State Protect Patients?
By Carrie Teegardin
Atlantic Journal-Constitution
A series on Physicians and Abuse
Here is an excerpt:
In most states, doctors dominate medical licensing boards and have the authority to decide who is fit to practice medicine and who isn’t. Usually the laws do not restrict a board’s authority by mandating certain punishments for some types of violations. Many licensing boards — including Georgia’s — say that’s how it should be.
“Having a bold, bright line saying a felony equals this or that is not good policy,” said Bob Jeffery, executive director of the Georgia Composite Medical Board.
Jeffery said criminal courts punish offenders and civil courts can compensate victims. Medical regulators, he said, have a different role.
“A licensing board is charged with making sure a (doctor) is safe to practice and that patients are protected,” he said.
With no legal prohibition standing in the way in most states, doctor-dominated medical boards often decide that doctors busted for abusive or illegal behaviors can be rehabilitated and safely returned to exam rooms.
New Jersey licensed a doctor convicted of sexual offenses with four patients. Kansas licensed a doctor imprisoned in Ohio for a sexual offense involving a child; that doctor later lost his Kansas license after making anonymous obscene phone calls to patients. Utah licensed a doctor who didn’t contest misdemeanor charges of sexual battery for intentionally touching the genitals of patients, staff members and others.
The article is here.
Atlantic Journal-Constitution
A series on Physicians and Abuse
Here is an excerpt:
In most states, doctors dominate medical licensing boards and have the authority to decide who is fit to practice medicine and who isn’t. Usually the laws do not restrict a board’s authority by mandating certain punishments for some types of violations. Many licensing boards — including Georgia’s — say that’s how it should be.
“Having a bold, bright line saying a felony equals this or that is not good policy,” said Bob Jeffery, executive director of the Georgia Composite Medical Board.
Jeffery said criminal courts punish offenders and civil courts can compensate victims. Medical regulators, he said, have a different role.
“A licensing board is charged with making sure a (doctor) is safe to practice and that patients are protected,” he said.
With no legal prohibition standing in the way in most states, doctor-dominated medical boards often decide that doctors busted for abusive or illegal behaviors can be rehabilitated and safely returned to exam rooms.
New Jersey licensed a doctor convicted of sexual offenses with four patients. Kansas licensed a doctor imprisoned in Ohio for a sexual offense involving a child; that doctor later lost his Kansas license after making anonymous obscene phone calls to patients. Utah licensed a doctor who didn’t contest misdemeanor charges of sexual battery for intentionally touching the genitals of patients, staff members and others.
The article is here.
Monday, July 11, 2016
Facebook has a new process for discussing ethics. But is it ethical?
Anna Lauren Hoffman
The Guardian
Originally posted Friday 17 June 2016
Here is an excerpt:
Tellingly, Facebook’s descriptions of procedure and process offer little insight into the values and ideals that drive its decision-making. Instead, the authors offer vague, hollow and at times conflicting statements such as noting how its reviewers “consider how the research will improve our society, our community, and Facebook”.
This seemingly innocuous statement raises more ethical questions than it answers. What does Facebook think an “improved” society looks like? Who or what constitutes “our community?” What values inform their ideas of a better society?
Facebook sidesteps this completely by saying that ethical oversight necessarily involves subjectivity and a degree of discretion on the part of reviewers – yet simply noting that subjectivity is unavoidable does not negate the fact that explicit discussion of ethical values is important.
The article is here.
The Guardian
Originally posted Friday 17 June 2016
Here is an excerpt:
Tellingly, Facebook’s descriptions of procedure and process offer little insight into the values and ideals that drive its decision-making. Instead, the authors offer vague, hollow and at times conflicting statements such as noting how its reviewers “consider how the research will improve our society, our community, and Facebook”.
This seemingly innocuous statement raises more ethical questions than it answers. What does Facebook think an “improved” society looks like? Who or what constitutes “our community?” What values inform their ideas of a better society?
Facebook sidesteps this completely by saying that ethical oversight necessarily involves subjectivity and a degree of discretion on the part of reviewers – yet simply noting that subjectivity is unavoidable does not negate the fact that explicit discussion of ethical values is important.
The article is here.
Wednesday, March 16, 2016
Bill would allow therapists to refuse clients over religious beliefs
Holly Meyer
The Tennessean
Originally published March 2, 2016
A bill that would allow counselors and therapists to refuse to see clients whose cases violate their religious beliefs has taken a step forward in the Tennessee state House.
The bill, sponsored by Rep. Dan Howell, R-Georgetown, would let counselors and therapists refer clients without risking repercussions, such as a civil lawsuit or criminal action. The state House Health Subcommittee advanced the legislation Tuesday to the full committee.
The subcommittee recommended passage of the legislation with an amendment that changes the bill's language from "sincerely held religious beliefs" to "sincerely held principles."
The article is here.
The Tennessean
Originally published March 2, 2016
A bill that would allow counselors and therapists to refuse to see clients whose cases violate their religious beliefs has taken a step forward in the Tennessee state House.
The bill, sponsored by Rep. Dan Howell, R-Georgetown, would let counselors and therapists refer clients without risking repercussions, such as a civil lawsuit or criminal action. The state House Health Subcommittee advanced the legislation Tuesday to the full committee.
The subcommittee recommended passage of the legislation with an amendment that changes the bill's language from "sincerely held religious beliefs" to "sincerely held principles."
The article is here.
Tuesday, January 12, 2016
Your Cells. Their Research. Your Permission?
By Rebecca Skloot
The New York Times
Originally posted December 30, 2015
Here are two excerpts:
What’s riding on this? Maybe the future of human health. We’re in the era of precision medicine, which relies on genetic and other personal information to develop individualized treatments. Those advances depend on scientists working with vast amounts of human tissue and DNA. Dr. Francis S. Collins, director of the National Institutes of Health, believes involving donors in this process gives scientists more useful information, and can be life-changing for donors. In announcing plans for the $215 million Precision Medicine Initiative, which he sees as a model for other future research, Dr. Collins said, “Participants will be partners in research, not subjects.” But people can be partners only if they know they’re participating.
(cut)
People have told me by the thousands, and numerous public opinion studies find the same: They want to know if their biospecimens are used in research, and they want to be asked first. Most will probably say yes, because they understand it’s important. They just don’t want to find out later. That damages their trust in science and doctors. It makes them wonder, what else are you hiding from me?
People tell me this because I wrote a book about Henrietta Lacks, a black tobacco farmer whose cancer cells, taken without her knowledge in 1951, are still alive in laboratories worldwide. Those cells, code-named HeLa, were the first such cells grown and one of the most important advances in medicine. But they came with troubling consequences: Her children were later used in research, their medical information was published, and the HeLa genome — including personal information about Mrs. Lacks and potentially her descendants — was sequenced and posted online. All without the family’s knowledge.
The article is here.
The New York Times
Originally posted December 30, 2015
Here are two excerpts:
What’s riding on this? Maybe the future of human health. We’re in the era of precision medicine, which relies on genetic and other personal information to develop individualized treatments. Those advances depend on scientists working with vast amounts of human tissue and DNA. Dr. Francis S. Collins, director of the National Institutes of Health, believes involving donors in this process gives scientists more useful information, and can be life-changing for donors. In announcing plans for the $215 million Precision Medicine Initiative, which he sees as a model for other future research, Dr. Collins said, “Participants will be partners in research, not subjects.” But people can be partners only if they know they’re participating.
(cut)
People have told me by the thousands, and numerous public opinion studies find the same: They want to know if their biospecimens are used in research, and they want to be asked first. Most will probably say yes, because they understand it’s important. They just don’t want to find out later. That damages their trust in science and doctors. It makes them wonder, what else are you hiding from me?
People tell me this because I wrote a book about Henrietta Lacks, a black tobacco farmer whose cancer cells, taken without her knowledge in 1951, are still alive in laboratories worldwide. Those cells, code-named HeLa, were the first such cells grown and one of the most important advances in medicine. But they came with troubling consequences: Her children were later used in research, their medical information was published, and the HeLa genome — including personal information about Mrs. Lacks and potentially her descendants — was sequenced and posted online. All without the family’s knowledge.
The article is here.
Friday, November 28, 2014
Therapist and Patient Share a Theater of Hurt
By Corey Kilgannon
The New York Times
Originally published November 5, 2014
Here is an excerpt:
Dr. Dintino said that her behavioral approach to Ms. Powell’s condition allows for a more personal relationship with the patient than conventional psychotherapy, and for looser guidelines when it comes to patient-therapist relations.
Ms. Powell was willing to bare all as a patient, and both women felt the risks were outweighed by the potential therapeutic value, as well as the attention that the show could bring to the disorder.
As for the notion that the decision constitutes a breach of ethics, Dr. Landy said, “With certain forms of mental illness that do not respond to conventional treatment, we need a more radical approach, which therapeutic theater can provide.”
The entire article is here.
The New York Times
Originally published November 5, 2014
Here is an excerpt:
Dr. Dintino said that her behavioral approach to Ms. Powell’s condition allows for a more personal relationship with the patient than conventional psychotherapy, and for looser guidelines when it comes to patient-therapist relations.
Ms. Powell was willing to bare all as a patient, and both women felt the risks were outweighed by the potential therapeutic value, as well as the attention that the show could bring to the disorder.
As for the notion that the decision constitutes a breach of ethics, Dr. Landy said, “With certain forms of mental illness that do not respond to conventional treatment, we need a more radical approach, which therapeutic theater can provide.”
The entire article is here.
Wednesday, November 5, 2014
Podcast Episode 17: Existential Angst, Ethics and Your Professional Will
Are you a psychologist working independently? If so, do you have a professional will? If not, you need to listen to this podcast. John welcomes Drs. Mary O’Leary Wiley and Cathy Spayd to outline the important points in constructing a professional will. A professional will is part of your ethical obligation to your patients should you die suddenly or become incapacitated. The podcast will address the pragmatics of constructing a professional will and why it is important for all psychologists to have a professional will.
At the end of the workshop the participants will be able to:
1. Explain the importance of a professional will.
2. Locate documents on the Internet to help create a professional will.
3. Create your professional will.
Click here to earn one APA-approved CE credit
Find this podcast on iTunes
Or listen directly below
**Some Corrective Feeback
- Some states require a public notification for practice closure, whatever the reason.
- Some psychologist's estates have been sued for failing to manage records properly after the death of a psychologist.
Resources
Mary O'Leary Wiley, PhD ABPP web site
Catherine Spayd, PhD
Closing a Professional Practice: Clinical, Ethical and Practical Considerations for Psychologists Throughout the Lifespan PowerPoint presentation by Drs. Wiley and Spayd
APA Sample of a Professional Will
Ragusea, S. (2002). A professional living will for psychologists and other mental health professionals. In L. VandeCreek & T. Jackson (Eds.), Innovations in clinical practice: A source book (Vol. 20, pp. 301 – 305). Sarasota, FL: Professional Resource Press.
Spayd, C.S. and Wiley, M.O. (2009). Closing a Professional Practice: Clinical and Practical Considerations. Pennsylvania Psychologist, 69 (11), 15-17.
Dashlane.com - A secure site to store passwords
At the end of the workshop the participants will be able to:
1. Explain the importance of a professional will.
2. Locate documents on the Internet to help create a professional will.
3. Create your professional will.
Find this podcast on iTunes
Or listen directly below
**Some Corrective Feeback
- Some states require a public notification for practice closure, whatever the reason.
- Some psychologist's estates have been sued for failing to manage records properly after the death of a psychologist.
Resources
Mary O'Leary Wiley, PhD ABPP web site
Catherine Spayd, PhD
Closing a Professional Practice: Clinical, Ethical and Practical Considerations for Psychologists Throughout the Lifespan PowerPoint presentation by Drs. Wiley and Spayd
APA Sample of a Professional Will
Ragusea, S. (2002). A professional living will for psychologists and other mental health professionals. In L. VandeCreek & T. Jackson (Eds.), Innovations in clinical practice: A source book (Vol. 20, pp. 301 – 305). Sarasota, FL: Professional Resource Press.
Spayd, C.S. and Wiley, M.O. (2009). Closing a Professional Practice: Clinical and Practical Considerations. Pennsylvania Psychologist, 69 (11), 15-17.
Dashlane.com - A secure site to store passwords
Monday, August 11, 2014
Episode 13: Ethics Education and Vignette Analysis (Number 2)
Lucky Episode 13 mirrors Episode 6 in that the content is similar. In the first half of the program, John speaks with Dr. Donald McAleer, psychologist and ethics educator, and his pre-doctoral intern Reneh Karamians about ethics education in graduate programs and at internship sites. We sprinkle in personal experience and the Acculturation Model focusing on how students and early career psychologists may think about ethical decision-making. In the second half, the participants discuss Vignette #5, A Tricky Situation from the "Vignette Warehouse" at the Ethics and Psychology site. Dr. McAleer and Intern Reneh arrive at different conclusions as to how to handle the vignette, which nicely models that there can be more than one right answer when dealing with ethical dilemmas.
At the end of this podcast, the listener will be able to:
1. Outline two important components in ethics education,
2. Identify the competing ethical principles in the vignette, and,
3. Practice integrating personal values with professional ethics.
Click here to earn one APA-approved CE credit
At the end of this podcast, the listener will be able to:
1. Outline two important components in ethics education,
2. Identify the competing ethical principles in the vignette, and,
3. Practice integrating personal values with professional ethics.
Click here to earn one APA-approved CE credit
Or listen directly below
Information on Dr. Don McAleer's Practice and Associated Pre-Doc Internship
Erie Psychological Consortium
Northshore Psychological Associates
Contact Don McAleer, PsyD, ABPP by email
Relevant Resources for this Podcast
Episode 4: Ethical Decision-making Part 1
Episode 5: Ethical Decision-making Part 2
Nonrational Processes in Ethical Decision-making
Mark Rogerson, Michael C. Gottlieb Mitchell M. Handelsman Samuel Knapp & Jeffrey Younggren
Beauchamp, T.L. & Childress, J.F. (1994). Principles of biomedical ethics ( 4th ed). New York: Oxford University Press.
Kitchener, K. S. (1984). Intuition, critical evaluation and ethical principles: The foundation for ethical decisions in counseling psychology. Counseling Psychologist, 12(3), 43-55.
Information on Dr. Don McAleer's Practice and Associated Pre-Doc Internship
Erie Psychological Consortium
Northshore Psychological Associates
Contact Don McAleer, PsyD, ABPP by email
Relevant Resources for this Podcast
Episode 4: Ethical Decision-making Part 1
Episode 5: Ethical Decision-making Part 2
Nonrational Processes in Ethical Decision-making
Mark Rogerson, Michael C. Gottlieb Mitchell M. Handelsman Samuel Knapp & Jeffrey Younggren
Beauchamp, T.L. & Childress, J.F. (1994). Principles of biomedical ethics ( 4th ed). New York: Oxford University Press.
Kitchener, K. S. (1984). Intuition, critical evaluation and ethical principles: The foundation for ethical decisions in counseling psychology. Counseling Psychologist, 12(3), 43-55.
Monday, March 17, 2014
Episode 4: Ethical Decision-making (Part 1)
While John's introduction indicates the podcasts will be conversations, Episode 4 is a monologue. This episode provides didactic material about ethical decision-making, which does not lend itself to a conversation. The importance of this podcast and Episode 5 is to set up vignette analysis in future podcasts. Everyone needs to be on the same page in order to apply ethical decision-making in instructional or real life situations.
At the end of this podcast, the listener will be able to:
1. Describe the differences between ethical and clinical decision-making,
2. Outline the Acculturation Model, and,
3. List the five foundational principles for ethical decision-making.
Click here to purchase 1 APA-approved Continuing Education credit
Find this podcast in iTunes
Listen directly on this page
Link to video presentation on YouTube
Here is a link to the PowerPoint presentation only.
Resources
American Psychological Association's Ethical Principles of Psychologists and Code of Conduct
American Psychological Association's Guidelines for Practitioners
Beauchamp, T.L. & Childress, J.F. (1994). Principles of biomedical ethics ( 4th ed). New York: Oxford University Press.
Kitchener, K. S. (1984). Intuition, critical evaluation and ethical principles: The foundation for ethical decisions in counseling psychology. Counseling Psychologist, 12(3), 43-55.
Handelsman, M. M., Gottlieb, M. C., & Knapp, S. (2005). Training ethical psychologists: An acculturation model. Professional Psychology: Research and Practice, 36, 59-65.
At the end of this podcast, the listener will be able to:
1. Describe the differences between ethical and clinical decision-making,
2. Outline the Acculturation Model, and,
3. List the five foundational principles for ethical decision-making.
Click here to purchase 1 APA-approved Continuing Education credit
Find this podcast in iTunes
Listen directly on this page
Link to video presentation on YouTube
Here is a link to the PowerPoint presentation only.
Resources
American Psychological Association's Ethical Principles of Psychologists and Code of Conduct
American Psychological Association's Guidelines for Practitioners
Beauchamp, T.L. & Childress, J.F. (1994). Principles of biomedical ethics ( 4th ed). New York: Oxford University Press.
Kitchener, K. S. (1984). Intuition, critical evaluation and ethical principles: The foundation for ethical decisions in counseling psychology. Counseling Psychologist, 12(3), 43-55.
Handelsman, M. M., Gottlieb, M. C., & Knapp, S. (2005). Training ethical psychologists: An acculturation model. Professional Psychology: Research and Practice, 36, 59-65.
Subscribe to:
Posts (Atom)