Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000–11
Nordt, Carlos et al.
The Lancet Psychiatry
DOI: http://dx.doi.org/10.1016/S2215-0366(14)00118-7
Summary
Background
As with previous economic downturns, there has been debate about an association between the 2008 economic crisis, rising unemployment, and suicide. Unemployment directly affects individuals' health and, unsurprisingly, studies have proposed an association between unemployment and suicide. However, a statistical model examining the relationship between unemployment and suicide by considering specific time trends among age-sex-country subgroups over wider world regions is still lacking. We aimed to enhance knowledge of the specific effect of unemployment on suicide by analysing global public data classified according to world regions.
Methods
We retrospectively analysed public data for suicide, population, and economy from the WHO mortality database and the International Monetary Fund's world economic outlook database from 2000 to 2011. We selected 63 countries based on sample size and completeness of the respective data and extracted the information about four age groups and sex. To check stability of findings, we conducted an overall random coefficient model including all study countries and four additional models, each covering a different world region.
Findings
Despite differences in the four world regions, the overall model, adjusted for the unemployment rate, showed that the annual relative risk of suicide decreased by 1·1% (95% CI 0·8–1·4) per year between 2000 and 2011. The best and most stable final model indicated that a higher suicide rate preceded a rise in unemployment (lagged by 6 months) and that the effect was non-linear with higher effects for lower baseline unemployment rates. In all world regions, the relative risk of suicide associated with unemployment was elevated by about 20–30% during the study period. Overall, 41 148 (95% CI 39 552–42 744) suicides were associated with unemployment in 2007 and 46 131 (44 292–47 970) in 2009, indicating 4983 excess suicides since the economic crisis in 2008.
Interpretation
Suicides associated with unemployment totalled a nine-fold higher number of deaths than excess suicides attributed to the most recent economic crisis. Prevention strategies focused on the unemployed and on employment and its conditions are necessary not only in difficult times but also in times of stable economy.
Welcome to the Nexus of Ethics, Psychology, Morality, Philosophy and Health Care
Welcome to the nexus of ethics, psychology, morality, technology, health care, and philosophy
Showing posts with label Access to Mental Health Services. Show all posts
Showing posts with label Access to Mental Health Services. Show all posts
Monday, March 9, 2015
Sunday, February 1, 2015
More Americans Getting Mental Health Treatment
By Deborah Brauser
MedScape
Originally published January 27, 2015
Behavioral health in the United States appears to be improving, especially for those between the ages of 12 and 17 years, a new report suggests.
The latest national behavioral health barometer from the Substance Abuse and Mental Health Services Administration (SAMHSA) showed that treatment for adults with mental illness increased from 62.9% in 2012 to 68.5% 1 year later. Substance use treatment for all age groups also increased significantly.
The entire article is here.
MedScape
Originally published January 27, 2015
Behavioral health in the United States appears to be improving, especially for those between the ages of 12 and 17 years, a new report suggests.
The latest national behavioral health barometer from the Substance Abuse and Mental Health Services Administration (SAMHSA) showed that treatment for adults with mental illness increased from 62.9% in 2012 to 68.5% 1 year later. Substance use treatment for all age groups also increased significantly.
The entire article is here.
Thursday, January 29, 2015
Is My Work “Medically Necessary”?
How insurance companies try to get around rules for mental health care.
By Darcy Lockman
Slate
Originally published January 12, 2015
Here is an excerpt:
I’ve been in private practice since 2010. Most of the people I see submit their bills to their insurance companies for reimbursement. It’s a testament to the integrity in the industry that these reimbursements often come through without a hitch. (Though only in this era of predictable corporate malfeasance could a company simply making good on its contractual obligations be praised for its integrity.) Somehow, four entire years went by during which I never once had to submit to a utilization review. But in the past year, possibly because of increased cost concerns in the wake of the Affordable Care Act, I’ve received a handful of phone calls, each caller requesting that I schedule a talk with a case manager.
The entire article is here.
By Darcy Lockman
Slate
Originally published January 12, 2015
Here is an excerpt:
I’ve been in private practice since 2010. Most of the people I see submit their bills to their insurance companies for reimbursement. It’s a testament to the integrity in the industry that these reimbursements often come through without a hitch. (Though only in this era of predictable corporate malfeasance could a company simply making good on its contractual obligations be praised for its integrity.) Somehow, four entire years went by during which I never once had to submit to a utilization review. But in the past year, possibly because of increased cost concerns in the wake of the Affordable Care Act, I’ve received a handful of phone calls, each caller requesting that I schedule a talk with a case manager.
The entire article is here.
Monday, January 26, 2015
Kaiser's 2,600 mental health workers strike in California
By Olga R. Rodriguez
AP via Yahoo News
Originally published January 13, 2014
Kaiser Permanente mental health professionals throughout California went on a strike Monday to protest what they say is a lack of staffing that affects care.
The health care provider's 2,600 psychologists, therapists and social workers began the weeklong walkout to demand that Kaiser Permanente offer timely, quality mental health care at its psychiatry departments and clinics, said Jim Clifford, a union member and San Diego psychiatric therapist.
Clifford said some patients have to wait up to two months for follow-up appointments, which prolongs the recovery process.
The entire article is here.
AP via Yahoo News
Originally published January 13, 2014
Kaiser Permanente mental health professionals throughout California went on a strike Monday to protest what they say is a lack of staffing that affects care.
The health care provider's 2,600 psychologists, therapists and social workers began the weeklong walkout to demand that Kaiser Permanente offer timely, quality mental health care at its psychiatry departments and clinics, said Jim Clifford, a union member and San Diego psychiatric therapist.
Clifford said some patients have to wait up to two months for follow-up appointments, which prolongs the recovery process.
The entire article is here.
Wednesday, January 21, 2015
Getting mental health services can be hard, despite law requiring parity
By Lisa Gillespie
The Washington Post
Originally published January 5, 2015
Even though more Americans than before have access to health insurance because of the Affordable Care Act, getting mental health services can still be challenging.
A report released in November concludes that despite a 2008 mental health parity law, some state exchange health plans may have a way to go to even the playing field between mental and physical benefits. The report, released by the advocacy group Mental Health America, was paid for by Takeda Pharmaceuticals U.S.A. and Lundbeck U.S.A., a pharmaceutical company that specializes in neurology and psychiatric treatments.
The report listed the states with the lowest prevalence of mental illness and the highest rates of access to care as Massachusetts, Vermont, Maine, North Dakota and Delaware. Those with the highest prevalence of mental illness and most limited access are Arizona, Mississippi, Nevada, Washington and Louisiana.
The entire article is here.
The Washington Post
Originally published January 5, 2015
Even though more Americans than before have access to health insurance because of the Affordable Care Act, getting mental health services can still be challenging.
A report released in November concludes that despite a 2008 mental health parity law, some state exchange health plans may have a way to go to even the playing field between mental and physical benefits. The report, released by the advocacy group Mental Health America, was paid for by Takeda Pharmaceuticals U.S.A. and Lundbeck U.S.A., a pharmaceutical company that specializes in neurology and psychiatric treatments.
The report listed the states with the lowest prevalence of mental illness and the highest rates of access to care as Massachusetts, Vermont, Maine, North Dakota and Delaware. Those with the highest prevalence of mental illness and most limited access are Arizona, Mississippi, Nevada, Washington and Louisiana.
The entire article is here.
Monday, November 24, 2014
More action sought to stop suicide in Canada
Suicide’s death toll exceeds homicide, and car accidents combined: the equivalent of ‘20 jumbo jets just disappearing.’
By Olivia Carville
The Star
Originally published on November 3, 2014
Every year, more Canadians kill themselves than die by car accidents, HIV, homicide, drowning, influenza and war combined.
In Ontario alone, the suicide rate doubles the road toll most years, figures obtained from the Office of the Chief Coroner show.
Despite this, preventive awareness campaigns and funding for suicide pales in comparison to all other public safety issues, experts told the Star.
The entire story is here.
By Olivia Carville
The Star
Originally published on November 3, 2014
Every year, more Canadians kill themselves than die by car accidents, HIV, homicide, drowning, influenza and war combined.
In Ontario alone, the suicide rate doubles the road toll most years, figures obtained from the Office of the Chief Coroner show.
Despite this, preventive awareness campaigns and funding for suicide pales in comparison to all other public safety issues, experts told the Star.
The entire story is here.
Sunday, October 26, 2014
The Internet, Suicide, & How Sites Like PostSecret Can Help
Studies show the Internet fails suicidal users. PostSecret shows how to help.
by Jennifer Golbeck, Ph.D.
Psychology Today Blog
Originally published October 4, 2014
People suffering from depression can feel isolated, lonely, and in need of help. As with so many other areas, the Internet is a natural place to turn for support. But, as with so many other things, the Internet is not always safe.
William Melchert-Dinkel, a former nurse who lives in Minnesota, was convicted last month for assisting the suicide of a British man online. Melchert-Dinkel spent his time visiting suicide-related internet forums where he posed as a suicidal female nurse. He would offer people step-by-step instructions on how to kill themselves (usually by hanging), and in ten cases, he entered into suicide pacts with other forum members. He believes five of those people went through with the suicides. In some cases, he may have watched people commit suicide over a webcam.
The entire blog post is here.
by Jennifer Golbeck, Ph.D.
Psychology Today Blog
Originally published October 4, 2014
People suffering from depression can feel isolated, lonely, and in need of help. As with so many other areas, the Internet is a natural place to turn for support. But, as with so many other things, the Internet is not always safe.
William Melchert-Dinkel, a former nurse who lives in Minnesota, was convicted last month for assisting the suicide of a British man online. Melchert-Dinkel spent his time visiting suicide-related internet forums where he posed as a suicidal female nurse. He would offer people step-by-step instructions on how to kill themselves (usually by hanging), and in ten cases, he entered into suicide pacts with other forum members. He believes five of those people went through with the suicides. In some cases, he may have watched people commit suicide over a webcam.
The entire blog post is here.
Sunday, October 12, 2014
The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care
Patrick W. Corrigan, Benjamin G. Druss, and Deborah A. Perlick
Psychological Science in the Public Interest 2014, Vol. 15(2) 37–70.
Summary
Treatments have been developed and tested to successfully reduce the symptoms and disabilities of many mental illnesses. Unfortunately, people distressed by these illnesses often do not seek out services or choose to fully engage in them. One factor that impedes care seeking and undermines the service system is mental illness stigma. In this article, we review the complex elements of stigma in order to understand its impact on participating in care. We then summarize public policy considerations in seeking to tackle stigma in order to improve treatment engagement. Stigma is a complex construct that includes public, self, and structural components. It directly affects people with mental illness, as well as their support system, provider network, and community resources. The effects of stigma are moderated by knowledge of mental illness and cultural relevance. Understanding stigma is central to reducing its negative impact on care seeking and treatment engagement. Separate strategies have evolved for counteracting the effects of public, self, and structural stigma. Programs for mental health providers may be especially fruitful for promoting care engagement. Mental health literacy, cultural competence, and family engagement campaigns also mitigate stigma’s adverse impact on care seeking. Policy change is essential to overcome the structural stigma that undermines government agendas meant to promote mental health care. Implications for expanding the research program on the connection between stigma and care seeking are discussed.
The entire article is here.
Psychological Science in the Public Interest 2014, Vol. 15(2) 37–70.
Summary
Treatments have been developed and tested to successfully reduce the symptoms and disabilities of many mental illnesses. Unfortunately, people distressed by these illnesses often do not seek out services or choose to fully engage in them. One factor that impedes care seeking and undermines the service system is mental illness stigma. In this article, we review the complex elements of stigma in order to understand its impact on participating in care. We then summarize public policy considerations in seeking to tackle stigma in order to improve treatment engagement. Stigma is a complex construct that includes public, self, and structural components. It directly affects people with mental illness, as well as their support system, provider network, and community resources. The effects of stigma are moderated by knowledge of mental illness and cultural relevance. Understanding stigma is central to reducing its negative impact on care seeking and treatment engagement. Separate strategies have evolved for counteracting the effects of public, self, and structural stigma. Programs for mental health providers may be especially fruitful for promoting care engagement. Mental health literacy, cultural competence, and family engagement campaigns also mitigate stigma’s adverse impact on care seeking. Policy change is essential to overcome the structural stigma that undermines government agendas meant to promote mental health care. Implications for expanding the research program on the connection between stigma and care seeking are discussed.
The entire article is here.
Thursday, October 2, 2014
Kaiser to pay $4 million fine over access to mental health services
By Cynthia H. Craft
Sacramento Bee
Originally posted September 10, 2014
Health care giant Kaiser Permanente has agreed to pay a $4 million fine to California’s overseer of managed health care following an 18-month battle with state officials over whether Kaiser blocked patients from timely access to mental health services.
(cut)
Moreover, the department found that Kaiser was likely violating state and federal mental health parity laws. The California Mental Health Parity Act requires managed care providers to provide psychiatric services that are equal in quality and access to their primary care services.
The entire article is here.
Sacramento Bee
Originally posted September 10, 2014
Health care giant Kaiser Permanente has agreed to pay a $4 million fine to California’s overseer of managed health care following an 18-month battle with state officials over whether Kaiser blocked patients from timely access to mental health services.
(cut)
Moreover, the department found that Kaiser was likely violating state and federal mental health parity laws. The California Mental Health Parity Act requires managed care providers to provide psychiatric services that are equal in quality and access to their primary care services.
The entire article is here.
Wednesday, September 17, 2014
Expansion of Mental Health Care Hits Obstacles
By Abby Goodnough
The New York Times
Originally published August 28, 2014
Here is an excerpt:
The new law is a big opportunity for mental health providers to reach more people of all income levels. But in Kentucky and the 25 other states that chose to expand Medicaid, the biggest expansion of mental health care has been for poor people who may have never had such treatment before.
Still, private providers face considerable headaches in taking on Medicaid patients, beyond the long-term deterrent of low reimbursement. Ms. Wright, for instance, is still waiting to be approved by some of the managed care companies that provide benefits to Medicaid recipients. Eager to build her client base, Ms. Wright has taken on a handful of new Medicaid enrollees for free while she waits for those companies to approve her paperwork.
“It’s been months and months,” she said. “It’s always there in my mind: Am I going to make it?”
The entire article is here.
The New York Times
Originally published August 28, 2014
Here is an excerpt:
The new law is a big opportunity for mental health providers to reach more people of all income levels. But in Kentucky and the 25 other states that chose to expand Medicaid, the biggest expansion of mental health care has been for poor people who may have never had such treatment before.
Still, private providers face considerable headaches in taking on Medicaid patients, beyond the long-term deterrent of low reimbursement. Ms. Wright, for instance, is still waiting to be approved by some of the managed care companies that provide benefits to Medicaid recipients. Eager to build her client base, Ms. Wright has taken on a handful of new Medicaid enrollees for free while she waits for those companies to approve her paperwork.
“It’s been months and months,” she said. “It’s always there in my mind: Am I going to make it?”
The entire article is here.
Friday, July 25, 2014
A new tactic to halt child abuse in Maryland
Focus now on helping low-risk families instead of punishing
By Yvonne Wenger
The Baltimore Sun
Originally posted July 5, 2014
Baltimore is changing the way it handles cases of alleged child abuse and neglect — part of a broad social-services strategy that has been touted by Maryland officials but abandoned in some other states.
The new approach, which is designed to lessen the adversarial relationship between families and caseworkers, puts cases on different tracks depending on whether they are deemed high or low risk. The tiered response, used in 23 states, is regarded as a best practice by many child advocates.
The entire story is here.
By Yvonne Wenger
The Baltimore Sun
Originally posted July 5, 2014
Baltimore is changing the way it handles cases of alleged child abuse and neglect — part of a broad social-services strategy that has been touted by Maryland officials but abandoned in some other states.
The new approach, which is designed to lessen the adversarial relationship between families and caseworkers, puts cases on different tracks depending on whether they are deemed high or low risk. The tiered response, used in 23 states, is regarded as a best practice by many child advocates.
The entire story is here.
Sunday, January 12, 2014
E.R. Costs for Mentally Ill Soar, and Hospitals Seek Better Way
By Julie Creswell
The New York Times
Originally published December 25, 2013
Here is an excerpt:
Today, North Carolina has only eight beds in state psychiatric hospitals per 100,000 people, the lowest ratio in the country.(North Carolina, like other states, has added beds in local community facilities but, even then, its total beds are down a quarter since 2001.)
Uninsured patients rarely receive individual therapy, only group sessions. And it can take up to three months to see a psychiatrist.
“Now, we are seeing some of the most acute, the most aggressive and the most chronic mental health patients, and we’re holding them longer,” said Janice Frohman, the director of WakeMed’s emergency department.
The effects of the upheaval in care of the mentally ill is playing out vividly at WakeMed. A private, nonprofit organization with 884 beds, WakeMed is struggling to find a way to meet the needs of increasing numbers of mentally ill patients while also controlling costs.
The entire article is here.
The New York Times
Originally published December 25, 2013
Here is an excerpt:
Today, North Carolina has only eight beds in state psychiatric hospitals per 100,000 people, the lowest ratio in the country.(North Carolina, like other states, has added beds in local community facilities but, even then, its total beds are down a quarter since 2001.)
Uninsured patients rarely receive individual therapy, only group sessions. And it can take up to three months to see a psychiatrist.
“Now, we are seeing some of the most acute, the most aggressive and the most chronic mental health patients, and we’re holding them longer,” said Janice Frohman, the director of WakeMed’s emergency department.
The effects of the upheaval in care of the mentally ill is playing out vividly at WakeMed. A private, nonprofit organization with 884 beds, WakeMed is struggling to find a way to meet the needs of increasing numbers of mentally ill patients while also controlling costs.
The entire article is here.
Saturday, December 14, 2013
People with mental health problems still waiting over a year for talking treatments, UK
Medical News Today
Originally published November 28, 2013
More than one in ten (12%) people with mental health problems are stuck on waiting lists for over a year before receiving talking treatments and over half (54%) wait over three months, reveals a new report launched by the We Need to Talk coalition of which the mental health charity Mind is part of (1).
The survey (2) of over 1,600 people who have tried to access talking therapies such as counselling and Cognitive Behaviour Therapy on the NHS in England over the last two years also shows how some people are paying for private therapy to get the help they desperately need. One in ten (11%) said that they had faced costs for private treatment because the therapy they needed was not available on the NHS.
The choice of treatment on offer was also found to be limited even though CBT, the most commonly prescribed talking treatment, doesn't work for everyone. The coalition found that three in five people (58%) weren't offered a choice in the type of therapy they received.
Since 2007, the Government's increased investment in the Improving Access to Psychological Therapies (IAPT) programme has helped millions of people to access psychological therapies on the NHS who otherwise wouldn't have had this support. However, delays in accessing support and a lack of choice is having a devastating effect on people's lives and recovery.
The entire article is here.
Originally published November 28, 2013
More than one in ten (12%) people with mental health problems are stuck on waiting lists for over a year before receiving talking treatments and over half (54%) wait over three months, reveals a new report launched by the We Need to Talk coalition of which the mental health charity Mind is part of (1).
The survey (2) of over 1,600 people who have tried to access talking therapies such as counselling and Cognitive Behaviour Therapy on the NHS in England over the last two years also shows how some people are paying for private therapy to get the help they desperately need. One in ten (11%) said that they had faced costs for private treatment because the therapy they needed was not available on the NHS.
The choice of treatment on offer was also found to be limited even though CBT, the most commonly prescribed talking treatment, doesn't work for everyone. The coalition found that three in five people (58%) weren't offered a choice in the type of therapy they received.
Since 2007, the Government's increased investment in the Improving Access to Psychological Therapies (IAPT) programme has helped millions of people to access psychological therapies on the NHS who otherwise wouldn't have had this support. However, delays in accessing support and a lack of choice is having a devastating effect on people's lives and recovery.
The entire article is here.
Saturday, November 9, 2013
Suicide Rate Climbs by 30 Percent in Kansas as Government Slashes Mental Health Budgets
Allison Kilkenny
on October 21, 2013
The Nation
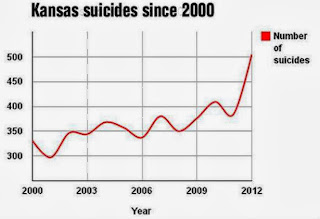 The Kansas
Department of Health and Environment recently released a startling report (PDF) showing
a 30 percent increase in suicides from 2011. Nationwide, the number of deaths
by suicide surpassed
the number of deaths by motor vehicle accidents in 2009, the
most recent year for which the Centers for Disease Control and Prevention
provided data.
The Kansas
Department of Health and Environment recently released a startling report (PDF) showing
a 30 percent increase in suicides from 2011. Nationwide, the number of deaths
by suicide surpassed
the number of deaths by motor vehicle accidents in 2009, the
most recent year for which the Centers for Disease Control and Prevention
provided data.The Wichita Eagle reports that the largest increase in suicides in Kansas occurred among white males, who already were the segment of the population most likely to take their own lives. More than 80 percent of suicides in Kansas last year were men, like Scott Dennis, a 42-year-old fitness company owner.
Wednesday, October 23, 2013
Professionalism and Caring for Medicaid Patients — The 5% Commitment?
Lawrence P. Casalino, M.D., Ph.D.
October 9, 2013 DOI: 10.1056/NEJMp1310974
Medicaid is an important federal–state partnership that provides health insurance for more than one fifth of the U.S. population — 73 million low-income people in 2012. The Affordable Care Act will expand Medicaid coverage to millions more. But 30% of office-based physicians do not accept new Medicaid patients, and in some specialties, the rate of nonacceptance is much higher — for example, 40% in orthopedics, 44% in general internal medicine, 45% in dermatology, and 56% in psychiatry. Physicians practicing in higher-income areas are less likely to accept new Medicaid patients. Physicians who do accept new Medicaid patients may use various techniques to severely limit their number — for example, one study of 289 pediatric specialty clinics showed that in the 34% of these clinics that accepted new Medicaid patients, the average waiting time for an appointment was 22 days longer for children on Medicaid than for privately insured children.
The entire story is here.
Thanks to Gary Schoener for this information.
October 9, 2013 DOI: 10.1056/NEJMp1310974
Medicaid is an important federal–state partnership that provides health insurance for more than one fifth of the U.S. population — 73 million low-income people in 2012. The Affordable Care Act will expand Medicaid coverage to millions more. But 30% of office-based physicians do not accept new Medicaid patients, and in some specialties, the rate of nonacceptance is much higher — for example, 40% in orthopedics, 44% in general internal medicine, 45% in dermatology, and 56% in psychiatry. Physicians practicing in higher-income areas are less likely to accept new Medicaid patients. Physicians who do accept new Medicaid patients may use various techniques to severely limit their number — for example, one study of 289 pediatric specialty clinics showed that in the 34% of these clinics that accepted new Medicaid patients, the average waiting time for an appointment was 22 days longer for children on Medicaid than for privately insured children.
The entire story is here.
Thanks to Gary Schoener for this information.
Monday, October 21, 2013
The New Asylums: Jails Swell With Mentally Ill
By Gary Fields and Ericka Phillips
The Wall Street Journal
Originally published September 25, 2013
Here is an excerpt:
America's lockups are its new asylums. After scores of state mental institutions were closed beginning in the 1970s, few alternatives materialized. Many of the afflicted wound up on the streets, where, untreated, they became more vulnerable to joblessness, drug abuse and crime.
The country's three biggest jail systems -- Cook County, in Illinois; Los Angeles County; and New York City -- are on the front lines. With more than 11,000 prisoners under treatment on any given day, they represent by far the largest mental-health treatment facilities in the country. By comparison, the three largest state-run mental hospitals have a combined 4,000 beds.
Put another way, the number of mentally ill prisoners the three facilities handle daily is equal to 28% of all beds in the nation's 213 state psychiatric hospitals, according to the National Association of State Mental Health Program Directors Research Institute Inc.
The entire story is here, hiding behind a paywall.
The Wall Street Journal
Originally published September 25, 2013
Here is an excerpt:
America's lockups are its new asylums. After scores of state mental institutions were closed beginning in the 1970s, few alternatives materialized. Many of the afflicted wound up on the streets, where, untreated, they became more vulnerable to joblessness, drug abuse and crime.
The country's three biggest jail systems -- Cook County, in Illinois; Los Angeles County; and New York City -- are on the front lines. With more than 11,000 prisoners under treatment on any given day, they represent by far the largest mental-health treatment facilities in the country. By comparison, the three largest state-run mental hospitals have a combined 4,000 beds.
Put another way, the number of mentally ill prisoners the three facilities handle daily is equal to 28% of all beds in the nation's 213 state psychiatric hospitals, according to the National Association of State Mental Health Program Directors Research Institute Inc.
The entire story is here, hiding behind a paywall.
Friday, October 11, 2013
Lacking Rules, Insurers Balk at Paying for Intensive Psychiatric Care
By REED ABELSON
The New York Times
Published: September 27, 2013
Here is an excerpt:
Melissa’s treatment did not come cheap: it ultimately cost hundreds of thousands of dollars, Ms. Morelli said. Patients often find themselves at odds with health insurers, but the battles are perhaps nowhere so heated as with the treatment of serious mental illness.
It was not supposed to be this way. A federal law, the Mental Health Parity and Addiction Equity Act of 2008, was aimed at avoiding fights like this over coverage by making sure insurers would cover mental illnesses just as they cover treatment for diseases like cancer or multiple sclerosis.
The entire story is here.
The New York Times
Published: September 27, 2013
Here is an excerpt:
Melissa’s treatment did not come cheap: it ultimately cost hundreds of thousands of dollars, Ms. Morelli said. Patients often find themselves at odds with health insurers, but the battles are perhaps nowhere so heated as with the treatment of serious mental illness.
It was not supposed to be this way. A federal law, the Mental Health Parity and Addiction Equity Act of 2008, was aimed at avoiding fights like this over coverage by making sure insurers would cover mental illnesses just as they cover treatment for diseases like cancer or multiple sclerosis.
The entire story is here.
Friday, October 4, 2013
Once Suicidal and Shipped Off, Now Battling Nevada Over Care
By RICK LYMAN
The New York Times
Published: September 21, 2013
Here is an excerpt:
But that is just a small sampling, Mr. Herrera says, of the estimated 1,500 people who were bused all over the country in recent years from the state-operated Rawson-Neal Psychiatric Center in Las Vegas and other Nevada institutions, 500 of them to California.
“It’s horrifying,” Mr. Herrera said. “I think we can all agree that our most vulnerable and at-risk people don’t deserve this sort of treatment: no meds, no medical care, a destination where they have no contacts and know no one.”
But what makes it “even more tragic,” Mr. Herrera said, “is that on top of the inhumane treatment, the State of Nevada was trying to have another jurisdiction shoulder the financial responsibility for caring for these people.”
The entire story is here.
Here is a prior story describing this practice.
The New York Times
Published: September 21, 2013
Here is an excerpt:
But that is just a small sampling, Mr. Herrera says, of the estimated 1,500 people who were bused all over the country in recent years from the state-operated Rawson-Neal Psychiatric Center in Las Vegas and other Nevada institutions, 500 of them to California.
“It’s horrifying,” Mr. Herrera said. “I think we can all agree that our most vulnerable and at-risk people don’t deserve this sort of treatment: no meds, no medical care, a destination where they have no contacts and know no one.”
But what makes it “even more tragic,” Mr. Herrera said, “is that on top of the inhumane treatment, the State of Nevada was trying to have another jurisdiction shoulder the financial responsibility for caring for these people.”
The entire story is here.
Here is a prior story describing this practice.
Tuesday, August 20, 2013
The Woman Who Ate Cutlery
By CHRISTINE MONTROSS
The New York Times - Opinion
Published: August 3, 2013
Here are some excerpts:
The costs of M’s repeated hospitalizations are staggering. Her ingestions and insertions incur the already high costs of hospital admission and the medical procedures and surgeries she requires. In addition, once M is hospitalized as a psychiatric patient, a staff member must stay with her at all times to make sure she doesn’t ingest utensils from her meal trays, insert tools from group craft activities into her body or drink Purell from the dispensers on the unit walls.
(cut)
In one of the ironies in a country with health care discrepancies, a single hospital admission for M — paid for by the taxpayer-financed state medical-assistance program — costs more than a year of private outpatient care would.
The entire article is here.
Thanks to Tom Fink for the story.
The New York Times - Opinion
Published: August 3, 2013
Here are some excerpts:
The costs of M’s repeated hospitalizations are staggering. Her ingestions and insertions incur the already high costs of hospital admission and the medical procedures and surgeries she requires. In addition, once M is hospitalized as a psychiatric patient, a staff member must stay with her at all times to make sure she doesn’t ingest utensils from her meal trays, insert tools from group craft activities into her body or drink Purell from the dispensers on the unit walls.
(cut)
In one of the ironies in a country with health care discrepancies, a single hospital admission for M — paid for by the taxpayer-financed state medical-assistance program — costs more than a year of private outpatient care would.
The entire article is here.
Thanks to Tom Fink for the story.
Wednesday, July 31, 2013
Most U.S. Health Spending Is Exploding — but Not for Mental Health
By Catherine Rampell
The New York Times Blog - Economix
Originally published July 2, 2013
Here is an excerpt:
Mental health spending, both public and private, was about $150 billion in 2009, more than double its level in inflation-adjusted terms in 1986, according to a recent article in Health Affairs. But the overall economy also about doubled during that time. As a result, direct mental health spending has remained roughly 1 percent of the economy since 1986, while total health spending climbed from about 10 percent of gross domestic product in 1986 to nearly 17 percent in 2009.
Thanks to Vince Bellwoar for this story.
Subscribe to:
Posts (Atom)