 Aono, D., Yaffe, G. & Kober, H.
Aono, D., Yaffe, G. & Kober, H.Cogn. Research 4, 40 (2019)
doi:10.1186/s41235-019-0179-y
Abstract
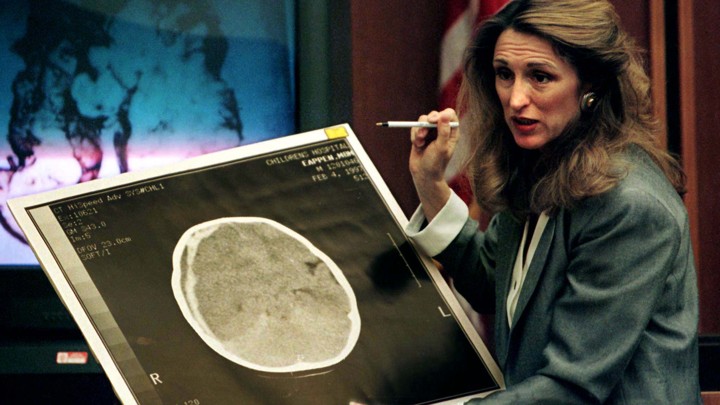
The use of neuroscience in the courtroom can be traced back to the early twentieth century. However, the use of neuroscientific evidence in criminal proceedings has increased significantly over the last two decades. This rapid increase has raised questions, among the media as well as the legal and scientific communities, regarding the effects that such evidence could have on legal decision makers. In this article, we first outline the history of neuroscientific evidence in courtrooms and then we provide a review of recent research investigating the effects of neuroscientific evidence on decision-making broadly, and on legal decisions specifically. In the latter case, we review studies that measure the effect of neuroscientific evidence (both imaging and nonimaging) on verdicts, sentencing recommendations, and beliefs of mock jurors and judges presented with a criminal case. Overall, the reviewed studies suggest mitigating effects of neuroscientific evidence on some legal decisions (e.g., the death penalty). Furthermore, factors such as mental disorder diagnoses and perceived dangerousness might moderate the mitigating effect of such evidence. Importantly, neuroscientific evidence that includes images of the brain does not appear to have an especially persuasive effect (compared with other neuroscientific evidence that does not include an image). Future directions for research are discussed, with a specific call for studies that vary defendant characteristics, the nature of the crime, and a juror’s perception of the defendant, in order to better understand the roles of moderating factors and cognitive mediators of persuasion.
Significance
The increased use of neuroscientific evidence in criminal proceedings has led some to wonder what effects such evidence has on legal decision makers (e.g., jurors and judges) who may be unfamiliar with neuroscience. There is some concern that legal decision makers may be unduly influenced by testimony and images related to the defendant’s brain. This paper briefly reviews the history of neuroscientific evidence in the courtroom to provide context for its current use. It then reviews the current research examining the influence of neuroscientific evidence on legal decision makers and potential moderators of such effects. Our synthesis of the findings suggests that neuroscientific evidence has some mitigating effects on legal decisions, although neuroimaging-based evidence does not hold any special persuasive power. With this in mind, we provide recommendations for future research in this area. Our review and conclusions have implications for scientists, legal scholars, judges, and jurors, who could all benefit from understanding the influence of neuroscientific evidence on judgments in criminal cases.

