Radley Balko and Tucker Carrington
The Washington Post
Originally posted March 21, 2018
Here is an excerpt:
At the trial level, juries hear far too much dubious science, whether it’s an unproven field like bite mark matching or blood splatter analysis, exaggerated claims in a field like hair fiber analysis, or analysts testifying outside their area of expertise. It’s difficult to say how many convictions have involved faulty or suspect forensics, but the FBI estimated in 2015 that its hair fiber analysts had testified in about 3,000 cases — and that’s merely one subspecialty of forensics, and only at the federal level. Extrapolating from the database of DNA exonerations, the Innocence Project estimates that bad forensics contributes to about 45 percent of wrongful convictions.
But flawed evidence presented at trial is only part of the problem. Even once a field of forensics or a particular expert has been discredited, the courts have made it extremely difficult for those convicted by bad science to get a new trial.
The Supreme Court makes judges responsible for determining what is good science. They already decide what evidence is allowed at trial, so asking them to do the same for expert testimony may seem intuitive. But judges are trained to do legal analyses, not scientific ones. They generally deal with challenges to expert testimony by looking at what other judges have said. If a previous court has allowed a field of forensic evidence, subsequent courts will, too.
The article is here.
Note: These issues also apply to psychologists in the courtroom.
Welcome to the Nexus of Ethics, Psychology, Morality, Philosophy and Health Care
Welcome to the nexus of ethics, psychology, morality, technology, health care, and philosophy
Showing posts with label Ethics and Law. Show all posts
Showing posts with label Ethics and Law. Show all posts
Monday, April 23, 2018
Tuesday, March 13, 2018
Doctors In Maine Say Halt In OxyContin Marketing Comes '20 Years Late'
Patty Wight
npr.org
Originally posted February 13, 2018
The maker of OxyContin, one of the most prescribed and aggressively marketed opioid painkillers, will no longer tout the drug or any other opioids to doctors.
The announcement, made Saturday, came as drugmaker Purdue Pharma faces lawsuits for deceptive marketing brought by cities and counties across the U.S., including several in Maine. The company said it's cutting its U.S. sales force by more than half.
Just how important are these steps against the backdrop of a raging opioid epidemic that took the lives of more than 300 Maine residents in 2016, and accounted for more than 42,000 deaths nationwide?
"They're 20 years late to the game," says Dr. Noah Nesin, a family physician and vice president of medical affairs at Penobscot Community Health Care.
Nesin says even after Purdue Pharma paid $600 million in fines about a decade ago for misleading doctors and regulators about the risks opioids posed for addiction and abuse, it continued marketing them.
The article is here.
npr.org
Originally posted February 13, 2018
The maker of OxyContin, one of the most prescribed and aggressively marketed opioid painkillers, will no longer tout the drug or any other opioids to doctors.
The announcement, made Saturday, came as drugmaker Purdue Pharma faces lawsuits for deceptive marketing brought by cities and counties across the U.S., including several in Maine. The company said it's cutting its U.S. sales force by more than half.
Just how important are these steps against the backdrop of a raging opioid epidemic that took the lives of more than 300 Maine residents in 2016, and accounted for more than 42,000 deaths nationwide?
"They're 20 years late to the game," says Dr. Noah Nesin, a family physician and vice president of medical affairs at Penobscot Community Health Care.
Nesin says even after Purdue Pharma paid $600 million in fines about a decade ago for misleading doctors and regulators about the risks opioids posed for addiction and abuse, it continued marketing them.
The article is here.
Monday, January 8, 2018
Advocacy group raises concerns about psychological evaluations on hundreds of defendants
Keith L. Alexander
The Washington Post
Originally published December 14, 2017
A District employee who has conducted mental evaluations on hundreds of criminal defendants as a forensic psychologist has been removed from that role after concerns surfaced about her educational qualifications, according to city officials.
Officials with the District’s Department of Health said Reston N. Bell was not qualified to conduct the assessments without the help or review of a supervisor. The city said it had mistakenly granted Bell, who was hired in 2016, a license to practice psychology, but this month the license was downgraded to “psychology associate.”
Although Bell has a master’s degree in psychology and a doctorate in education, she does not have a PhD in psychology, which led to the downgrade.
The article is here.
The Washington Post
Originally published December 14, 2017
A District employee who has conducted mental evaluations on hundreds of criminal defendants as a forensic psychologist has been removed from that role after concerns surfaced about her educational qualifications, according to city officials.
Officials with the District’s Department of Health said Reston N. Bell was not qualified to conduct the assessments without the help or review of a supervisor. The city said it had mistakenly granted Bell, who was hired in 2016, a license to practice psychology, but this month the license was downgraded to “psychology associate.”
Although Bell has a master’s degree in psychology and a doctorate in education, she does not have a PhD in psychology, which led to the downgrade.
The article is here.
Monday, December 18, 2017
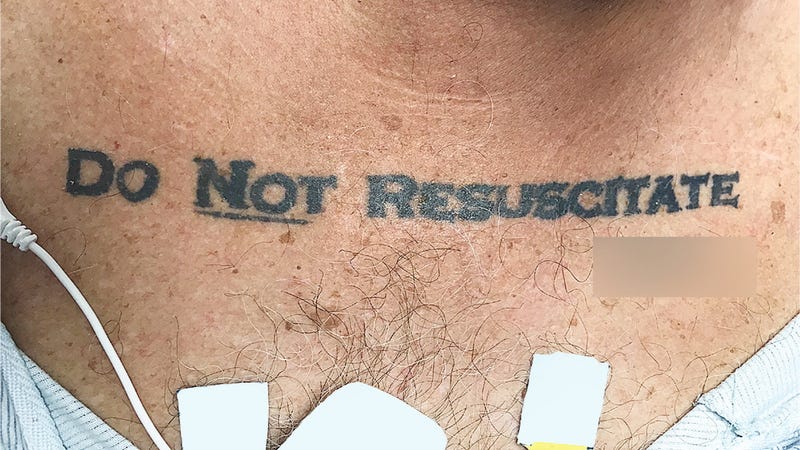
Unconscious Patient With 'Do Not Resuscitate' Tattoo Causes Ethical Conundrum at Hospital
George Dvorsky
Gizmodo
Originally published November 30, 2017
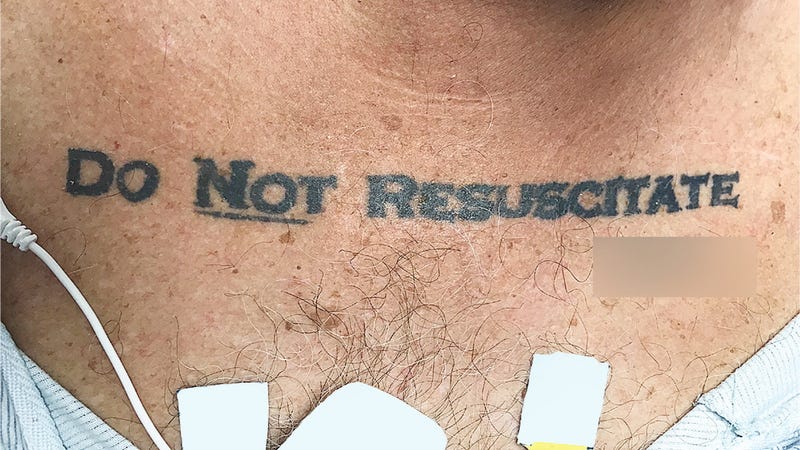 When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.
When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.
But with the “DO NOT RESUSCITATE” tattoo glaring back at them, the ICU team was suddenly confronted with a serious dilemma. The patient arrived at the hospital without ID, the medical staff was unable to contact next of kin, and efforts to revive or communicate with the patient were futile. The medical staff had no way of knowing if the tattoo was representative of the man’s true end-of-life wishes, so they decided to play it safe and ignore it.
The article is here.
Gizmodo
Originally published November 30, 2017
 When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.
When an unresponsive patient arrived at a Florida hospital ER, the medical staff was taken aback upon discovering the words “DO NOT RESUSCITATE” tattooed onto the man’s chest—with the word “NOT” underlined and with his signature beneath it. Confused and alarmed, the medical staff chose to ignore the apparent DNR request—but not without alerting the hospital’s ethics team, who had a different take on the matter.But with the “DO NOT RESUSCITATE” tattoo glaring back at them, the ICU team was suddenly confronted with a serious dilemma. The patient arrived at the hospital without ID, the medical staff was unable to contact next of kin, and efforts to revive or communicate with the patient were futile. The medical staff had no way of knowing if the tattoo was representative of the man’s true end-of-life wishes, so they decided to play it safe and ignore it.
The article is here.
Friday, September 15, 2017
Robots and morality
The Big Read (which is actually in podcast form)
The Financial Times
Originally posted August 2017
Now our mechanical creations can act independently, what happens when AI goes wrong? Where does moral, ethical and legal responsibility for robots lie — with the manufacturers, the programmers, the users or the robots themselves, asks John Thornhill. And who owns their rights?
Click on the link below to access the 13 minutes podcast.
Podcast is here.
The Financial Times
Originally posted August 2017
Now our mechanical creations can act independently, what happens when AI goes wrong? Where does moral, ethical and legal responsibility for robots lie — with the manufacturers, the programmers, the users or the robots themselves, asks John Thornhill. And who owns their rights?
Click on the link below to access the 13 minutes podcast.
Podcast is here.
Monday, September 11, 2017
Nonvoluntary Psychiatric Treatment Is Distinct From Involuntary Psychiatric Treatment
Dominic A. Sisti
JAMA. Published online August 24, 2017
Some of the most ethically challenging cases in mental health care involve providing treatment to individuals who refuse that treatment. Sometimes when persons with mental illness become unsafe to themselves or others, they must be taken, despite their outward and often vigorous refusal, to an emergency department or psychiatric hospital to receive treatment, such as stabilizing psychotropic medication. On occasion, to provide medical care over objection, a patient must be physically restrained.
The modifier “involuntary” is generally used to describe these cases. For example, it is said that a patient has been involuntarily hospitalized or is receiving involuntary medication ostensibly because the patient did not consent and was forced or strongly coerced into treatment. Importantly, a person may be involuntarily hospitalized but retain the right to refuse treatment. “Involuntary” is also used to describe instances when an individual is committed to outpatient treatment by a court. The fact that a person is being treated involuntarily raises numerous challenges; it raises concerns about protecting individual liberty, respect for patient autonomy, and the specter of past abuses of patients in psychiatric institutions.
Although it has become both a clinical colloquialism and legal touchstone, the concept of involuntary treatment is used imprecisely to describe all instances in which a patient has refused the treatment he or she subsequently receives. In some cases, a patient outwardly refuses treatment but may have previously expressed a desire to be treated in crisis or, according to a reasonable evaluator, he or she would have agreed to accept stabilizing treatment, such as antipsychotic medication. A similar scenario occurs in the treatment of individuals who experience a first episode of psychosis and who outwardly refuse treatment. With no prior experience of what it is like to have psychosis, these patients are unable to develop informed preferences about treatment in advance of their first crisis. In these cases, some believe it is reasonable to provide treatment despite the opposition of the patient, although this could be debated.
The article is here.
JAMA. Published online August 24, 2017
Some of the most ethically challenging cases in mental health care involve providing treatment to individuals who refuse that treatment. Sometimes when persons with mental illness become unsafe to themselves or others, they must be taken, despite their outward and often vigorous refusal, to an emergency department or psychiatric hospital to receive treatment, such as stabilizing psychotropic medication. On occasion, to provide medical care over objection, a patient must be physically restrained.
The modifier “involuntary” is generally used to describe these cases. For example, it is said that a patient has been involuntarily hospitalized or is receiving involuntary medication ostensibly because the patient did not consent and was forced or strongly coerced into treatment. Importantly, a person may be involuntarily hospitalized but retain the right to refuse treatment. “Involuntary” is also used to describe instances when an individual is committed to outpatient treatment by a court. The fact that a person is being treated involuntarily raises numerous challenges; it raises concerns about protecting individual liberty, respect for patient autonomy, and the specter of past abuses of patients in psychiatric institutions.
Although it has become both a clinical colloquialism and legal touchstone, the concept of involuntary treatment is used imprecisely to describe all instances in which a patient has refused the treatment he or she subsequently receives. In some cases, a patient outwardly refuses treatment but may have previously expressed a desire to be treated in crisis or, according to a reasonable evaluator, he or she would have agreed to accept stabilizing treatment, such as antipsychotic medication. A similar scenario occurs in the treatment of individuals who experience a first episode of psychosis and who outwardly refuse treatment. With no prior experience of what it is like to have psychosis, these patients are unable to develop informed preferences about treatment in advance of their first crisis. In these cases, some believe it is reasonable to provide treatment despite the opposition of the patient, although this could be debated.
The article is here.
Wednesday, September 6, 2017
The Nuremberg Code 70 Years Later
Jonathan D. Moreno, Ulf Schmidt, and Steve Joffe
JAMA. Published online August 17, 2017.
Seventy years ago, on August 20, 1947, the International Medical Tribunal in Nuremberg, Germany, delivered its verdict in the trial of 23 doctors and bureaucrats accused of war crimes and crimes against humanity for their roles in cruel and often lethal concentration camp medical experiments. As part of its judgment, the court articulated a 10-point set of rules for the conduct of human experiments that has come to be known as the Nuremberg Code. Among other requirements, the code called for the “voluntary consent” of the human research subject, an assessment of risks and benefits, and assurances of competent investigators. These concepts have become an important reference point for the ethical conduct of medical research. Yet, there has in the past been considerable debate among scholars about the code’s authorship, scope, and legal standing in both civilian and military science. Nonetheless, the Nuremberg Code has undoubtedly been a milestone in the history of biomedical research ethics.1- 3
Writings on medical ethics, laws, and regulations in a number of jurisdictions and countries, including a detailed and sophisticated set of guidelines from the Reich Ministry of the Interior in 1931, set the stage for the code. The same focus on voluntariness and risk that characterizes the code also suffuses these guidelines. What distinguishes the code is its context. As lead prosecutor Telford Taylor emphasized, although the Doctors’ Trial was at its heart a murder trial, it clearly implicated the ethical practices of medical experimenters and, by extension, the medical profession’s relationship to the state understood as an organized community living under a particular political structure. The embrace of Nazi ideology by German physicians, and the subsequent participation of some of their most distinguished leaders in the camp experiments, demonstrates the importance of professional independence from and resistance to the ideological and geopolitical ambitions of the authoritarian state.
The article is here.
JAMA. Published online August 17, 2017.
Seventy years ago, on August 20, 1947, the International Medical Tribunal in Nuremberg, Germany, delivered its verdict in the trial of 23 doctors and bureaucrats accused of war crimes and crimes against humanity for their roles in cruel and often lethal concentration camp medical experiments. As part of its judgment, the court articulated a 10-point set of rules for the conduct of human experiments that has come to be known as the Nuremberg Code. Among other requirements, the code called for the “voluntary consent” of the human research subject, an assessment of risks and benefits, and assurances of competent investigators. These concepts have become an important reference point for the ethical conduct of medical research. Yet, there has in the past been considerable debate among scholars about the code’s authorship, scope, and legal standing in both civilian and military science. Nonetheless, the Nuremberg Code has undoubtedly been a milestone in the history of biomedical research ethics.1- 3
Writings on medical ethics, laws, and regulations in a number of jurisdictions and countries, including a detailed and sophisticated set of guidelines from the Reich Ministry of the Interior in 1931, set the stage for the code. The same focus on voluntariness and risk that characterizes the code also suffuses these guidelines. What distinguishes the code is its context. As lead prosecutor Telford Taylor emphasized, although the Doctors’ Trial was at its heart a murder trial, it clearly implicated the ethical practices of medical experimenters and, by extension, the medical profession’s relationship to the state understood as an organized community living under a particular political structure. The embrace of Nazi ideology by German physicians, and the subsequent participation of some of their most distinguished leaders in the camp experiments, demonstrates the importance of professional independence from and resistance to the ideological and geopolitical ambitions of the authoritarian state.
The article is here.
Tuesday, August 22, 2017
Informed-consent ruling may have “far-reaching, negative impact”
Andis Robeznieks
AMA Wire
Originally published August 8, 2017
Here are two excerpts:
A lawsuit alleging Dr. Toms had not obtained informed consent was initiated by Shinal and her husband on Dec. 17, 2009. The brief notes that Shinal “did not assert that the harm was the result of negligence” and that “there is no contention” that Dr. Toms’ staff provided inaccurate information during the informed consent process.
A jury found for Dr. Toms. Shinal appealed and the Pennsylvania Superior Court affirmed the decision. The case was heard before the Pennsylvania Supreme Court in November 2016. The case was decided June 20.
According to Wecht, a key issue is “whether the trial court misapplied the common law and the MCARE Act when it instructed the jury that it could consider information provided to Mrs. Shinal by Dr. Toms' ‘qualified staff’ in deciding whether Dr. Toms obtained Mrs. Shinal's informed consent to aggressive brain surgery.”
(cut)
PAMED General Counsel Angela Boateng also weighed in.
“It was not uncommon for other qualified staff to assist a physician in providing the requisite information or answering follow-up questions a patient may have had. The Medical Practice Act and other professional regulations permitted this level of assistance,” she commented. “The patient’s ability to follow up with the physician or his qualified staff was usually aimed at promoting a patient’s understanding of the treatment or procedure to be completed. The court’s decision, however, has put an end to this practice.”
The article is here.
AMA Wire
Originally published August 8, 2017
Here are two excerpts:
A lawsuit alleging Dr. Toms had not obtained informed consent was initiated by Shinal and her husband on Dec. 17, 2009. The brief notes that Shinal “did not assert that the harm was the result of negligence” and that “there is no contention” that Dr. Toms’ staff provided inaccurate information during the informed consent process.
A jury found for Dr. Toms. Shinal appealed and the Pennsylvania Superior Court affirmed the decision. The case was heard before the Pennsylvania Supreme Court in November 2016. The case was decided June 20.
According to Wecht, a key issue is “whether the trial court misapplied the common law and the MCARE Act when it instructed the jury that it could consider information provided to Mrs. Shinal by Dr. Toms' ‘qualified staff’ in deciding whether Dr. Toms obtained Mrs. Shinal's informed consent to aggressive brain surgery.”
(cut)
PAMED General Counsel Angela Boateng also weighed in.
“It was not uncommon for other qualified staff to assist a physician in providing the requisite information or answering follow-up questions a patient may have had. The Medical Practice Act and other professional regulations permitted this level of assistance,” she commented. “The patient’s ability to follow up with the physician or his qualified staff was usually aimed at promoting a patient’s understanding of the treatment or procedure to be completed. The court’s decision, however, has put an end to this practice.”
The article is here.
Saturday, August 12, 2017
Reminder: the Trump International Hotel is still an ethics disaster
Carly Sitrin
Vox.com
Originally published August 8, 2017
The Trump International Hotel in Washington, DC, has been serving as a White House extension since Donald Trump took office, and experts think this violates several governmental ethics rules.
The Washington Post reported Monday that the Trump International Hotel has played host to countless foreign dignitaries, Republican lawmakers, and powerful actors hoping to hold court with Trump appointees or even the president himself.
Since visitation records at the Trump International Hotel are not made public, the Post sent reporters to the hotel every day in May to try to identify people and organizations using the facilities.
What they found was a revolving door of powerful people holding galas in the hotel’s lavish ballrooms and meeting over expensive cocktails with White House staff at the bar.
They included Rep. Dana Rohrabacher (R-CA), whom Politico recently called "Putin’s favorite congressman”; Rep. Bill Shuster (R-PA), who chairs the General Services Administration, the Trump hotel's landlord; and nine other Republican Congress members who all hosted events at the hotel, according to campaign spending disclosures obtained by the Post. Additionally, foreign visitors such as business groups promoting Turkish-American relations and the Romanian President Klaus Iohannis and his wife also rented out rooms.
The article is here.
Vox.com
Originally published August 8, 2017
The Trump International Hotel in Washington, DC, has been serving as a White House extension since Donald Trump took office, and experts think this violates several governmental ethics rules.
The Washington Post reported Monday that the Trump International Hotel has played host to countless foreign dignitaries, Republican lawmakers, and powerful actors hoping to hold court with Trump appointees or even the president himself.
Since visitation records at the Trump International Hotel are not made public, the Post sent reporters to the hotel every day in May to try to identify people and organizations using the facilities.
What they found was a revolving door of powerful people holding galas in the hotel’s lavish ballrooms and meeting over expensive cocktails with White House staff at the bar.
They included Rep. Dana Rohrabacher (R-CA), whom Politico recently called "Putin’s favorite congressman”; Rep. Bill Shuster (R-PA), who chairs the General Services Administration, the Trump hotel's landlord; and nine other Republican Congress members who all hosted events at the hotel, according to campaign spending disclosures obtained by the Post. Additionally, foreign visitors such as business groups promoting Turkish-American relations and the Romanian President Klaus Iohannis and his wife also rented out rooms.
The article is here.
Tuesday, July 18, 2017
Responding to whistleblower’s claims, Duke admits research data falsification
Ray Gronberg
The Herald-Sun
Originally published July 2, 2017
In-house investigators at Duke University believe a former lab tech falsified or fabricated data that went into 29 medical research reports, lawyers for the university say in their answer to a federal whistleblower lawsuit against it.
Duke’s admissions concern the work of Erin Potts-Kant, and a probe it began in 2013 when she was implicated in an otherwise-unrelated embezzlement. The lawsuit, from former lab analyst Joseph Thomas, contends Duke and some of its professors used the phony data to fraudulently obtain federal research grants. He also alleges they ignored warning signs about Potts-Kants’ work, and tried to cover up the fraud.
The university’s lawyers have tried to get the case dismissed, but in April, a federal judge said it can go ahead. The latest filings thus represent Duke’s first answer to the substance of Thomas’ allegations.
Up front, it said Potts-Kant told a Duke investigating committee that she’d faked data that wound up being “included in various publications and grant applications.”
The article is here.
The Herald-Sun
Originally published July 2, 2017
In-house investigators at Duke University believe a former lab tech falsified or fabricated data that went into 29 medical research reports, lawyers for the university say in their answer to a federal whistleblower lawsuit against it.
Duke’s admissions concern the work of Erin Potts-Kant, and a probe it began in 2013 when she was implicated in an otherwise-unrelated embezzlement. The lawsuit, from former lab analyst Joseph Thomas, contends Duke and some of its professors used the phony data to fraudulently obtain federal research grants. He also alleges they ignored warning signs about Potts-Kants’ work, and tried to cover up the fraud.
The university’s lawyers have tried to get the case dismissed, but in April, a federal judge said it can go ahead. The latest filings thus represent Duke’s first answer to the substance of Thomas’ allegations.
Up front, it said Potts-Kant told a Duke investigating committee that she’d faked data that wound up being “included in various publications and grant applications.”
The article is here.
Wednesday, July 5, 2017
DOJ corporate compliance watchdog resigns citing Trump's conduct
Olivia Beavers
The Hill
Originally published July 2, 2017
A top Justice Department official who serves as a corporate compliance watchdog has left her job, saying she felt she could no longer force companies to comply with the government's ethics laws when members of the administration she works for have conducted themselves in a manner that she claims would not be tolerated.
Hui Chen had served in the department’s compliance counsel office from November 2015 until she resigned in June, breaking her silence in a LinkedIn post last week highlighted by The International Business Times, which points to the Trump administration’s behavior as the reason for her job change.
“To sit across the table from companies and question how committed they were to ethics and compliance felt not only hypocritical, but very much like shuffling the deck chair on the Titanic," Chen wrote.
The article is here.
The Hill
Originally published July 2, 2017
A top Justice Department official who serves as a corporate compliance watchdog has left her job, saying she felt she could no longer force companies to comply with the government's ethics laws when members of the administration she works for have conducted themselves in a manner that she claims would not be tolerated.
Hui Chen had served in the department’s compliance counsel office from November 2015 until she resigned in June, breaking her silence in a LinkedIn post last week highlighted by The International Business Times, which points to the Trump administration’s behavior as the reason for her job change.
“To sit across the table from companies and question how committed they were to ethics and compliance felt not only hypocritical, but very much like shuffling the deck chair on the Titanic," Chen wrote.
The article is here.
Sunday, June 4, 2017
Physicians, Firearms, and Free Speech
Wendy E. Parmet, Jason A. Smith, and Matthew Miller
N Engl J Med 2017; 376:1901-1903
May 18, 2017
Here is an excerpt:
The majority’s well-reasoned decision, in fact, does just that. By relying on heightened rather than strict scrutiny, the majority affirmed that laws regulating physician speech must be designed to enhance rather than harm patient safety. The majority took this mandate seriously and required the state to show some meaningful evidence that the regulation was apt to serve the state’s interest in protecting patients.
The state could not do so for two reasons. First, the decision to keep a gun in the home substantially increases the risk of death for all household members, especially the risk of death by suicide, and particularly so when guns are stored loaded and unlocked, as they are in millions of homes where children live. Second, the majority of U.S. adults who live in homes with guns are unaware of the heightened risk posed by bringing guns into a home. Indeed, by providing accurate information about the risks created by easy access to firearms, as well as ways to modify that risk (e.g., by storing guns unloaded and locked up, separate from ammunition), a physician’s counseling can not only enhance a patient’s capacity for self-determination, but also save lives.
Given the right to provide such counsel, professional norms recognize the responsibility to do so. Fulfilling this obligation, however, may not be easy, since the chief impediments to doing so — and to doing so effectively — are not and never have been legal barriers. Indeed, the court’s welcome ruling does not ensure that most clinicians will honor this hard-won victory by exercising their First Amendment rights.
The article is here.
N Engl J Med 2017; 376:1901-1903
May 18, 2017
Here is an excerpt:
The majority’s well-reasoned decision, in fact, does just that. By relying on heightened rather than strict scrutiny, the majority affirmed that laws regulating physician speech must be designed to enhance rather than harm patient safety. The majority took this mandate seriously and required the state to show some meaningful evidence that the regulation was apt to serve the state’s interest in protecting patients.
The state could not do so for two reasons. First, the decision to keep a gun in the home substantially increases the risk of death for all household members, especially the risk of death by suicide, and particularly so when guns are stored loaded and unlocked, as they are in millions of homes where children live. Second, the majority of U.S. adults who live in homes with guns are unaware of the heightened risk posed by bringing guns into a home. Indeed, by providing accurate information about the risks created by easy access to firearms, as well as ways to modify that risk (e.g., by storing guns unloaded and locked up, separate from ammunition), a physician’s counseling can not only enhance a patient’s capacity for self-determination, but also save lives.
Given the right to provide such counsel, professional norms recognize the responsibility to do so. Fulfilling this obligation, however, may not be easy, since the chief impediments to doing so — and to doing so effectively — are not and never have been legal barriers. Indeed, the court’s welcome ruling does not ensure that most clinicians will honor this hard-won victory by exercising their First Amendment rights.
The article is here.
Saturday, May 13, 2017
Justices Blast One-Stop-Shop Experts in Alabama
Tim Ryan
Courthouse News
Originally posted April 24, 2017
The Supreme Court’s liberal justices shredded an argument by Alabama’s solicitor general Monday that criminal defendants are not entitled to a mental health expert separate from the ones tapped by prosecutors.
McWilliams v. Dunn, the case the Supreme Court heard this morning, is nested inside the court’s 1984 decision in Ake v. Oklahoma, which held that poor criminal defendants using a defense of insanity are entitled to an expert to help support their claim.
A split has emerged in the 30 years since the decision, with some states deciding one expert helping both the prosecution and defense satisfies the requirement, and others choosing to assign an expert for the defendant to use exclusively.
The article is here.
Courthouse News
Originally posted April 24, 2017
The Supreme Court’s liberal justices shredded an argument by Alabama’s solicitor general Monday that criminal defendants are not entitled to a mental health expert separate from the ones tapped by prosecutors.
McWilliams v. Dunn, the case the Supreme Court heard this morning, is nested inside the court’s 1984 decision in Ake v. Oklahoma, which held that poor criminal defendants using a defense of insanity are entitled to an expert to help support their claim.
A split has emerged in the 30 years since the decision, with some states deciding one expert helping both the prosecution and defense satisfies the requirement, and others choosing to assign an expert for the defendant to use exclusively.
The article is here.
Wednesday, May 10, 2017
How do you punish a criminal robot?
Christopher Markou
The Independent
Originally posted on April 20, 2017
Here is an excerpt:
Among the many things that must now be considered is what role and function the law will play. Expert opinions differ wildly on the likelihood and imminence of a future where sufficiently advanced robots walk among us, but we must confront the fact that autonomous technology with the capacity to cause harm is already around. Whether it’s a military drone with a full payload, a law enforcement robot exploding to kill a dangerous suspect or something altogether more innocent that causes harm through accident, error, oversight, or good ol’ fashioned stupidity.
There’s a cynical saying in law that “wheres there’s blame, there’s a claim”. But who do we blame when a robot does wrong? This proposition can easily be dismissed as something too abstract to worry about. But let’s not forget that a robot was arrested (and released without charge) for buying drugs; and Tesla Motors was absolved of responsibility by the American National Highway Traffic Safety Administration when a driver was killed in a crash after his Tesla was in autopilot.
While problems like this are certainly peculiar, history has a lot to teach us. For instance, little thought was given to who owned the sky before the Wright Brothers took the Kitty Hawk for a joyride. Time and time again, the law is presented with these novel challenges. And despite initial overreaction, it got there in the end. Simply put: law evolves.
The article is here.
The Independent
Originally posted on April 20, 2017
Here is an excerpt:
Among the many things that must now be considered is what role and function the law will play. Expert opinions differ wildly on the likelihood and imminence of a future where sufficiently advanced robots walk among us, but we must confront the fact that autonomous technology with the capacity to cause harm is already around. Whether it’s a military drone with a full payload, a law enforcement robot exploding to kill a dangerous suspect or something altogether more innocent that causes harm through accident, error, oversight, or good ol’ fashioned stupidity.
There’s a cynical saying in law that “wheres there’s blame, there’s a claim”. But who do we blame when a robot does wrong? This proposition can easily be dismissed as something too abstract to worry about. But let’s not forget that a robot was arrested (and released without charge) for buying drugs; and Tesla Motors was absolved of responsibility by the American National Highway Traffic Safety Administration when a driver was killed in a crash after his Tesla was in autopilot.
While problems like this are certainly peculiar, history has a lot to teach us. For instance, little thought was given to who owned the sky before the Wright Brothers took the Kitty Hawk for a joyride. Time and time again, the law is presented with these novel challenges. And despite initial overreaction, it got there in the end. Simply put: law evolves.
The article is here.
Who Decides When a Patient Can’t? Statutes on Alternate Decision Makers
Erin S. DeMartino and others
The New England Journal of Medicine
DOI: 10.1056/NEJMms1611497
Many patients cannot make their own medical decisions, having lost what is called decisional capacity. The estimated prevalence of decisional incapacity approaches 40% among adult medical
inpatients and residential hospice patients and exceeds 90% among adults in some intensive care
units.3,4 Patients who lack capacity may guide decisions regarding their own care through an
advance directive, a legal document that records treatment preferences or designates a durable
power of attorney for health care, or both. Unfortunately,the rate of completion of advance directives
in the general U.S. population hovers around 20 to 29%, creating uncertainty about who will
fill the alternate decision-maker role for many patients.
There is broad ethical consensus that other persons may make life-and-death decisions on
behalf of patients who lack decisional capacity. Over the past few decades, many states have enacted
legislation designed to delineate decisionmaking authority for patients who lack advance directives. Yet the 50 U.S. states and the District of Columbia vary in their procedures for appointing and challenging default surrogates, the attributes they require of such persons, their priority ranking of possible decision makers, and dispute resolution. These differences have important implications for clinicians, patients, and public health.
The article is here.
The New England Journal of Medicine
DOI: 10.1056/NEJMms1611497
Many patients cannot make their own medical decisions, having lost what is called decisional capacity. The estimated prevalence of decisional incapacity approaches 40% among adult medical
inpatients and residential hospice patients and exceeds 90% among adults in some intensive care
units.3,4 Patients who lack capacity may guide decisions regarding their own care through an
advance directive, a legal document that records treatment preferences or designates a durable
power of attorney for health care, or both. Unfortunately,the rate of completion of advance directives
in the general U.S. population hovers around 20 to 29%, creating uncertainty about who will
fill the alternate decision-maker role for many patients.
There is broad ethical consensus that other persons may make life-and-death decisions on
behalf of patients who lack decisional capacity. Over the past few decades, many states have enacted
legislation designed to delineate decisionmaking authority for patients who lack advance directives. Yet the 50 U.S. states and the District of Columbia vary in their procedures for appointing and challenging default surrogates, the attributes they require of such persons, their priority ranking of possible decision makers, and dispute resolution. These differences have important implications for clinicians, patients, and public health.
The article is here.
Tuesday, March 21, 2017
Why can 12-year-olds still get married in the United States?
Fraidy Reiss
The Washington Post
Originally published February 10, 2017
Here is an excerpt:
Unchained At Last, a nonprofit I founded to help women resist or escape forced marriage in the United States, spent the past year collecting marriage license data from 2000 to 2010, the most recent year for which most states were able to provide information. We learned that in 38 states, more than 167,000 children — almost all of them girls, some as young 12 — were married during that period, mostly to men 18 or older. Twelve states and the District of Columbia were unable to provide information on how many children had married there in that decade. Based on the correlation we identified between state population and child marriage, we estimated that the total number of children wed in America between 2000 and 2010 was nearly 248,000.
Despite these alarming numbers, and despite the documented consequences of early marriages, including negative effects on health and education and an increased likelihood of domestic violence, some state lawmakers have resisted passing legislation to end child marriage — because they wrongly fear that such measures might unlawfully stifle religious freedom or because they cling to the notion that marriage is the best solution for a teen pregnancy.
The article is here.
The Washington Post
Originally published February 10, 2017
Here is an excerpt:
Unchained At Last, a nonprofit I founded to help women resist or escape forced marriage in the United States, spent the past year collecting marriage license data from 2000 to 2010, the most recent year for which most states were able to provide information. We learned that in 38 states, more than 167,000 children — almost all of them girls, some as young 12 — were married during that period, mostly to men 18 or older. Twelve states and the District of Columbia were unable to provide information on how many children had married there in that decade. Based on the correlation we identified between state population and child marriage, we estimated that the total number of children wed in America between 2000 and 2010 was nearly 248,000.
Despite these alarming numbers, and despite the documented consequences of early marriages, including negative effects on health and education and an increased likelihood of domestic violence, some state lawmakers have resisted passing legislation to end child marriage — because they wrongly fear that such measures might unlawfully stifle religious freedom or because they cling to the notion that marriage is the best solution for a teen pregnancy.
The article is here.
Saturday, February 25, 2017
Sorry is Never Enough: The Effect of State Apology Laws on Medical Malpractice Liability Risk
Benjamin J. McMichaela, R. Lawrence Van Hornb, & W. Kip Viscusic
Abstract:
State apology laws offer a separate avenue from traditional damages-centric tort reforms to promote communication between physicians and patients and to address potential medical malpractice liability. These laws facilitate apologies from physicians by excluding statements of apology from malpractice trials. Using a unique dataset that includes all malpractice claims for 90% of physicians practicing in a single specialty across the country, this study examines whether apology laws limit malpractice risk. For physicians who do not regularly perform surgery, apology laws increase the probability of facing a lawsuit and increase the average payment made to resolve a claim. For surgeons, apology laws do not have a substantial effect on the probability of facing a claim or the average payment made to resolve a claim. Overall, the evidence suggests that apology laws do not effectively limit medical malpractice liability risk.
The article is here.
Abstract:
State apology laws offer a separate avenue from traditional damages-centric tort reforms to promote communication between physicians and patients and to address potential medical malpractice liability. These laws facilitate apologies from physicians by excluding statements of apology from malpractice trials. Using a unique dataset that includes all malpractice claims for 90% of physicians practicing in a single specialty across the country, this study examines whether apology laws limit malpractice risk. For physicians who do not regularly perform surgery, apology laws increase the probability of facing a lawsuit and increase the average payment made to resolve a claim. For surgeons, apology laws do not have a substantial effect on the probability of facing a claim or the average payment made to resolve a claim. Overall, the evidence suggests that apology laws do not effectively limit medical malpractice liability risk.
The article is here.
Wednesday, February 15, 2017
Judge Allows Lawsuit Against Psychologists in C.I.A. Torture Case
Sheri Fink
The New York Times
Originally published January 29, 2017
A federal judge on Friday allowed a case brought by former detainees to move forward against two American psychologists who helped devise the C.I.A.’s now-defunct program to interrogate terrorism suspects using techniques widely considered to be torture.
A United States District Court judge, Justin L. Quackenbush, denied a motion by the psychologists that sought to dismiss the case for lack of jurisdiction under provisions of a 2006 law that limits the ability of detainees to challenge their treatment.
“This ruling sends the strong signal that anyone who participates in shameful and unlawful government torture can’t count on escaping accountability in a court of law,” said Dror Ladin, a staff attorney for the American Civil Liberties Union, which, with the Gibbons law firm in Newark, represents the former detainees.
The article is here.
The New York Times
Originally published January 29, 2017
A federal judge on Friday allowed a case brought by former detainees to move forward against two American psychologists who helped devise the C.I.A.’s now-defunct program to interrogate terrorism suspects using techniques widely considered to be torture.
A United States District Court judge, Justin L. Quackenbush, denied a motion by the psychologists that sought to dismiss the case for lack of jurisdiction under provisions of a 2006 law that limits the ability of detainees to challenge their treatment.
“This ruling sends the strong signal that anyone who participates in shameful and unlawful government torture can’t count on escaping accountability in a court of law,” said Dror Ladin, a staff attorney for the American Civil Liberties Union, which, with the Gibbons law firm in Newark, represents the former detainees.
The article is here.
Wednesday, February 8, 2017
Medical culture encourages doctors to avoid admitting mistakes
By Lawrence Schlachter
STAT News
Originally published on January 13, 2017
Here are two excerpts:
In reality, the factor that most influences doctors to hide or disclose medical errors should be clear to anyone who has spent much time in the profession: The culture of medicine frowns on admitting mistakes, usually on the pretense of fear of malpractice lawsuits.
But what’s really at risk are doctors’ egos and the preservation of a system that lets physicians avoid accountability by ignoring problems or shifting blame to “the system” or any culprit other than themselves.
(cut)
What is a patient to do in this environment? The first thing is to be aware of your own predisposition to take everything your doctor says at face value. Listen closely and you may hear cause for more intense questioning.
You will likely never hear the terms negligence, error, mistake, or injury in a hospital. Instead, these harsh but truthful words and phrases are replaced with softer ones like accident, adverse event, or unfortunate outcome. If you hear any of these euphemisms, ask more questions or seek another opinion from a different doctor, preferably at a different facility.
Most doctors would never tell a flagrant lie. But in my experience as a neurosurgeon and as an attorney, too many of them resort to half-truths and glaring omissions when it comes to errors. Beware of passive language like “the patient experienced bleeding” rather than “I made a bad cut”; attributing an error to random chance or a nameless, faceless system; or trivialization of the consequences of the error by claiming something was “a blessing in disguise.”
The article is here.
STAT News
Originally published on January 13, 2017
Here are two excerpts:
In reality, the factor that most influences doctors to hide or disclose medical errors should be clear to anyone who has spent much time in the profession: The culture of medicine frowns on admitting mistakes, usually on the pretense of fear of malpractice lawsuits.
But what’s really at risk are doctors’ egos and the preservation of a system that lets physicians avoid accountability by ignoring problems or shifting blame to “the system” or any culprit other than themselves.
(cut)
What is a patient to do in this environment? The first thing is to be aware of your own predisposition to take everything your doctor says at face value. Listen closely and you may hear cause for more intense questioning.
You will likely never hear the terms negligence, error, mistake, or injury in a hospital. Instead, these harsh but truthful words and phrases are replaced with softer ones like accident, adverse event, or unfortunate outcome. If you hear any of these euphemisms, ask more questions or seek another opinion from a different doctor, preferably at a different facility.
Most doctors would never tell a flagrant lie. But in my experience as a neurosurgeon and as an attorney, too many of them resort to half-truths and glaring omissions when it comes to errors. Beware of passive language like “the patient experienced bleeding” rather than “I made a bad cut”; attributing an error to random chance or a nameless, faceless system; or trivialization of the consequences of the error by claiming something was “a blessing in disguise.”
The article is here.
Tuesday, February 7, 2017
Trump's Ethics Plan Is Even Worse Than You Thought
Timothy L. O'Brien
Bloomberg News
Originally posted February 6, 2017
Here is an excerpt:
The documents note that President Trump is to receive “exclusive benefit” from any assets in the trust. In other words, he still could see profits from the Trump Organization flow directly into his wallet and he gets to keep those for himself. While Donald Trump Jr. and Weisselberg have legal authority over the assets in the trust, the president can revoke their authority at any time.
How much money might course through the Trump Organization and find its way to the president may never be discernable because Trump has resisted releasing his tax returns ever since he began his White House bid. Keeping those returns buried is also out of step with presidential tradition. While Trump’s spokeswoman, Kellyanne Conway, has tried to minimize the significance of that lapse, Trump’s refusal to do so continues to concern voters.
Trump’s tax returns are significant -- they would offer the public a necessary window onto his business dealings, his philanthropic efforts, his overseas operations and the financial forces that will come to bear upon him in the White House. Yet Trump has latched on to a number of slender reasons for avoiding releasing them.
The article is here.
Bloomberg News
Originally posted February 6, 2017
Here is an excerpt:
The documents note that President Trump is to receive “exclusive benefit” from any assets in the trust. In other words, he still could see profits from the Trump Organization flow directly into his wallet and he gets to keep those for himself. While Donald Trump Jr. and Weisselberg have legal authority over the assets in the trust, the president can revoke their authority at any time.
How much money might course through the Trump Organization and find its way to the president may never be discernable because Trump has resisted releasing his tax returns ever since he began his White House bid. Keeping those returns buried is also out of step with presidential tradition. While Trump’s spokeswoman, Kellyanne Conway, has tried to minimize the significance of that lapse, Trump’s refusal to do so continues to concern voters.
Trump’s tax returns are significant -- they would offer the public a necessary window onto his business dealings, his philanthropic efforts, his overseas operations and the financial forces that will come to bear upon him in the White House. Yet Trump has latched on to a number of slender reasons for avoiding releasing them.
The article is here.
Subscribe to:
Posts (Atom)